- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
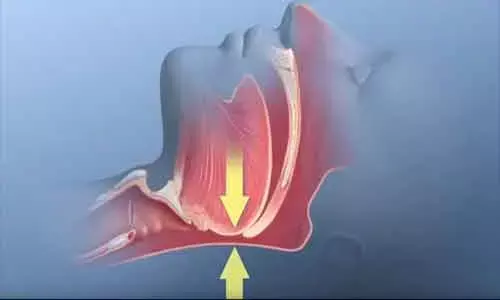
Non-CPAP therapies for obstructive sleep apnea: European Respiratory Society guidelines
Germany: Obstructive sleep apnoea (OSA) treatment in adults is evolving, as new therapies have been explored and introduced in clinical practice, while other approaches have been refined or reconsidered. A recent study published in the journal European Respiratory Review, reports European Respiratory Society guidelines on non-CPAP therapies for obstructive sleep apnoea (OSA). It is an update of the 2011 ERS statement on non-CPAP therapies, advanced into a clinical guideline.
The present recommendation was determined by a systematic review of the literature. For developing the guideline, a multidisciplinary group of experts generated eight key clinical questions and conducted a systematic review to identify published randomized clinical trials that answered these questions. The GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach was deployed to assess the quality of the evidence and the strength of recommendations.
The resulting guideline addresses gastric bypass surgery, custom-made dual-block mandibular advancement devices, hypoglossal nerve stimulation, myofunctional therapy, maxillo-mandibular osteotomy, carbonic anhydrase inhibitors, and positional therapy. These recommendations can be used to benchmark the quality of care for people with OSA across Europe and to improve outcomes.
Nine questions were formulated addressing patient, intervention, comparison, outcome (PICO) by telephone conferences. Given below are the questions with the developed recommendations.
PICO 1: In adult obese patients with OSA, should laparoscopic Roux-en-Y gastric bypass surgery or a weight-reducing diet be used?
Recommendation: In adult obese patients with OSA, the task force suggest bariatric surgery evaluation versus a weight-reducing diet when weight has not improved despite participating in a comprehensive weight reduction program and if there are no contraindications.
PICO 2: Should a custom-made dual-block mandibular advancement device or CPAP be used for adult patients with OSA?
Recommendation: In adult patients with OSA, the task force suggest that CPAP should be used as compared to MAD.
PICO 3: Should HNS during sleep or no treatment be used for adult patients with OSA?
Recommendation: The task force suggests that HNS should not be used as a first-line treatment for OSA patients in general (conditional recommendation, very low quality of evidence). However, we suggest that HNS compared to no treatment should be considered as a salvage treatment in patients with symptomatic OSA, who cannot be sufficiently treated with positive airway pressure treatment (CPAP, bilevel positive airway pressure) or MAD, and who have an AHI <50 events·h−1 and a BMI <32 kg·m−2.
PICO 4a: In adult patients with OSA, should myofunctional therapy or no treatment be used?
Recommendation: The task force does not suggest myofunctional therapy as a standard/regular treatment of OSA, but only for specific cases seeking alternative treatments and who are reluctant to undertake surgical or mechanical strategies.
PICO 4b: Should myofunctional therapy or CPAP be used for adult patients with OSA?
Recommendation: The task force suggests using CPAP instead of myofunctional therapy for adult patients.
PICO 5: Should maxillo-mandibular osteotomy or CPAP be used for adult patients with OSA?
Recommendation: In adult patients with OSA, the task force suggests using either MMO or CPAP.
PICO 6: Should carbonic anhydrase inhibitors (compared to placebo) be used for adult patients with OSA?
Recommendation: The task force suggest the use of carbonic anhydrase inhibitors only in the context of an RCT, as there is no drug in this category with an approved label for OSA.
PICO 7: Should positional therapy or CPAP be used for adult patients with position-dependent OSA?
Recommendation: The task force suggests either positional therapy using vibratory devices or CPAP among adult patients with mild or moderate position-dependent OSA as defined by a supine AHI at least twice as high as the nonsupine AHI and no relevant nonsupine AHI (<15 events·h−1).
PICO 8: Should positional therapy (intervention) or custom-made dual-block MADs (control) be used for adult patients with adult position-dependent OSA?
Recommendation: In patients with mild positional OSA, the task force suggests using either vibrational positional therapy or MAD.
Reference:
European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. Winfried Randerath, Johan Verbraecken, Christel A.L. de Raaff, Jan Hedner, Simon Herkenrath, Winfried Hohenhorst, Tina Jakob, Oreste Marrone, Marie Marklund, Walter T. McNicholas, Rebecca L. Morgan, Jean-Louis Pepin, Sofia Schiza, Nicole Skoetz, Dan Smyth, Jörg Steier, Thomy Tonia, Wojciech Trzepizur, Piet-Heijn van Mechelen, Peter Wijkstra. European Respiratory Review Dec 2021, 30 (162) 210200; DOI: 10.1183/16000617.0200-2021
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


