- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
CPAP helps lower blood sugar in diabetics with sleep apnea: Study
China: Patients with type 2 diabetes (T2D) and sleep apnea when treated with CPAP experience improved insulin resistance and blood sugar control, finds a recent study in the journal Diabetes, Obesity and Metabolism.
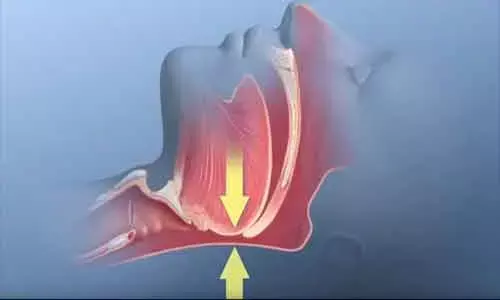
Obstructive sleep apnea (OSA) is a common chronic respiratory disorder characterized by sleep-induced recurrent upper airway collapse. After more than three decades from its first use, continuous positive airway pressure (CPAP) is still recognized as the gold standard treatment. In earlier studies, Sleep apnea has been linked with elevated blood sugar levels, suggesting people with the condition could be at an increased risk of cardiovascular illness and mortality.
Obstructive sleep apnea and T2D are two interacting epidemics and both have high prevalence and morbidity. Epidemiological and clinical studies have suggested that majority of T2D patients have OSA. Sleep apnea when untreated in these patients results in poor blood sugar control leading to acceleration of complications related to diabetes. CPAP is a non-pharmacological intervention which is the gold-standard treatment of OSA and is highly effective in relieving OSA symptoms and might be of benefit to diabetes patients too.
Wenli Shang, Shaanxi Provincial People's Hospital, Xi'an, Shaanxi, PR China, and colleagues performed the meta-analysis to determine the effects of continuous positive airway pressure (CPAP) treatment on insulin resistance and glycemic control in patients with T2D and obstructive sleep apnea.
The researchers performed systematic search of online databases and included randomized controlled trials (RCTs) on treatment of T2D and OSA with CPAP, compared with sham CPAP or no CPAP. Seven trials consisting of 691 participants met the inclusion criteria.
CPAP presented significant effects on glycated hemoglobin (HbA1c) (SMD ‐0.32), fasting glucose (SMD ‐0.39), Homeostasis Model Assessment‐Insulin Resistance (HOMA‐IR) (SMD ‐1.05), systolic blood pressure (SBP) (SMD ‐1.18), and diastolic blood pressure (DBP) (SMD ‐1.29).
"CPAP treatment significantly improved glycemic control and insulin resistance, indicated by the decreased levels of HbA1c, fasting glucose, and HOMA‐IR in patients with type 2 diabetes and contemporary OSA," concluded the authors.
"Benefits of CPAP on glycemic control and insulin resistance in patients with type 2 diabetes and obstructive sleep apnea: a meta‐analysis," is published in the journal Diabetes, Obesity and Metabolism.
DOI: https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/dom.14247
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


