- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
New technical approach can enhance diagnosis of pulmonary hypertension
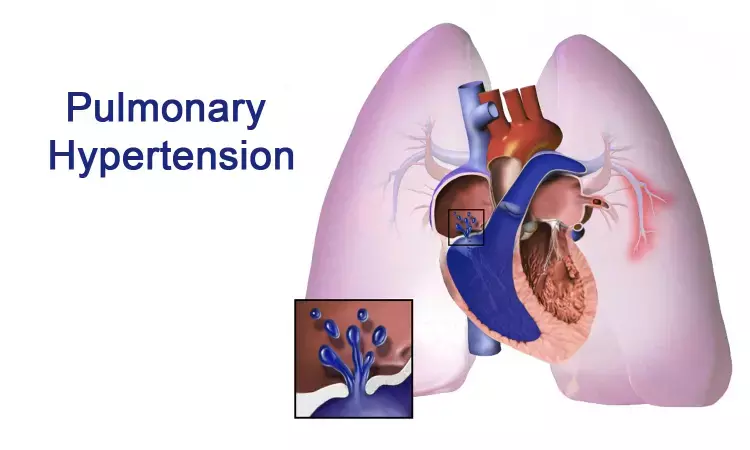
Molecular analysis may facilitate targeted treatment of pulmonary hypertension by differentiating underlying conditions affecting pulmonary arteries and veins, report scientists in The American Journal of Pathology.
Philadelphia – Pulmonary hypertension (PH) is a serious problem associated with a wide variety of lung diseases, which can lead to right ventricular dysfunction and death. Currently, there is no drug therapy to cure PH and the condition may necessitate lung transplantation. The management and prognosis of PH heavily relies on whether the pathology is localized in pulmonary arteries or veins. In particular, at early stages, it is challenging to distinguish pulmonary arterial hypertension (PAH) from the rare subtype of pulmonary veno-occlusive disease (PVOD) because clinical presentations of PAH and PVOD can be similar. A new study in The American Journal of Pathology, published by Elsevier, reports gene expression analysis of lung explant tissue can accurately differentiate PAH from PVOD.
"The pathogenesis of PVOD and PAH is poorly understood and the clinical differentiation between both diseases remains challenging because of similar clinical presentation," explained lead investigator Lavinia Neubert, MD, Institute of Pathology, Hannover Medical School, and Member of the German Center for Lung Research (DZL), Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), Hannover, Germany. "Our study is the first to put forward a molecular model with the ability to differentiate between the PH subtypes PAH and PVOD. Our findings promise to help develop novel target-specific interventions and innovative approaches to facilitate clinical diagnostics in an elusive group of diseases."
Patients with PH often experience narrowing, blockage, or destruction of lung blood vessels, a process referred to as vascular remodeling. In this study, researchers analyzed lung samples from patients with PAH, PVOD, idiopathic pulmonary fibrosis (IPF), chronic obstructive pulmonary disease (COPD), and healthy controls. As anticipated, patients with PAH had pathological changes predominantly in pulmonary arteries and arterioles, whereas samples from patients with PVOD were characterized by alterations of the post-capillary pulmonary vasculature (veins).
Caption: Hematoxilin-eosin staining of human formalin-fixed and paraffin-embedded lung tissue: Obliterated pulmonary artery in pulmonary arterial hypertension showing fibrosis of the intima, hypertrophy of the media, and plexiform vasculopathy in A. Occluded pulmonary vein in pulmonary veno-occlusive disease showing fibrosis of the intima and hypertrophy of the media in B. Scale bars are labeled with 200 µm. Credit: Institute of Pathology, Hannover Medical School, April 2020.
Using deep-learning algorithms to analyze the molecular findings, the researchers were able to successfully differentiate disease entities with 100 percent sensitivity and 92 percent specificity, based on six target genes. Interestingly, samples from PVOD patients shared more regulatory characteristics with samples from patients with IPF than with PAH.
"We are confident that the classification accuracy of our molecular approach is close to the gold standard, of histopathological diagnosis," said Dr. Neubert. "Since lung biopsies remain as high-risk interventions for PH patients and non-invasive approaches currently do not allow for a definite diagnostic accuracy, these findings may facilitate diagnosis of PVOD by molecular analysis, provided that our findings are reproducible in blood or urine samples."
Additional analyses using quantitative proteomics and multiplex immunohistochemistry identified a variety of dysregulated genes. Some of the gene changes were common to all patients with severe pulmonary vascular remodeling regardless of the afflicted lung compartments, while others were more specific.
The investigators believe genetic signaling changes in various forms of severe PH might serve as novel pharmaceutical targets with the potential to address severe vascular remodeling. They recommend further studies to investigate the diagnostic value of the identified markers in the clinical setting.
PH is a condition in which blood pressure from the heart to the lungs is higher than normal. Symptoms of PH include breathing impairment (dyspnea), chest pain, light-headedness, and weakness. Impaired gas exchange, right heart overload, and death by right heart failure result in high mortality and morbidity for those with PH. Medications, surgical interventions, and exercise may help control symptoms.
For further reference log on to:
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


