- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
School-Based Asthma Therapy improves Medicine adherence and asthma control among children: Study
Researchers have found in a new study that School-based asthma therapy significantly enhanced asthma control and medication adherence. This led to a notable reduction in healthcare utilization, including fewer emergency department (ED) visits and hospitalizations. Overall, Asthma Control Test (ACT) scores improved by 37%.
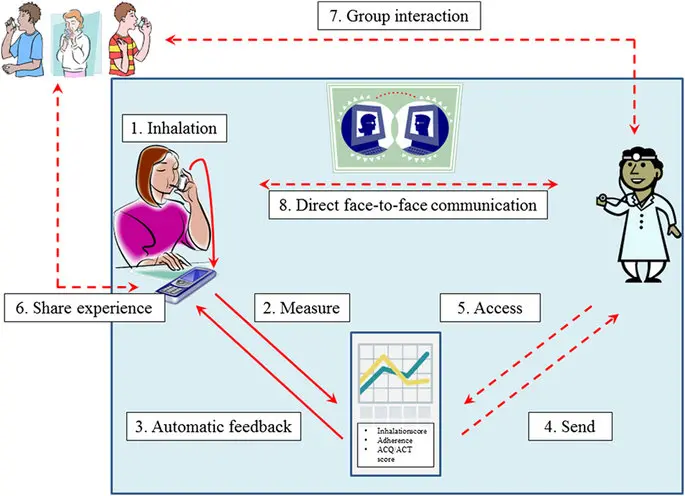
Undertreatment and poor adherence remain prevalent for children with persistent asthma. School-based asthma therapy (SBAT) provides guideline-based treatment by systematic school-based asthma screenings and direct administration of daily controller medications.
They examined asthma control and health care utilization for children enrolled in the SBAT program in Columbus, Ohio, from 2013 to 2019. Six-year retrospective medical records were reviewed for 1 year before and 1 year after SBAT enrollment for children aged 5 to 19 years from 2 metropolitan school districts. Asthma control was assessed by the Asthma Control Test (ACT) and health care provider (HCP) ratings. Information was collected regarding asthma-related health care utilization, including emergency department (ED), urgent care, and acute care visits; hospitalizations; and pediatric intensive care unit (PICU) admissions.
Results: Percentage increases in well-controlled asthma were 37% (ACT) and 56% (HCP). Asthma-related ED visits decreased by 49%, hospitalizations 50%, PICU admissions 71%, urgent care visits 41%, and acute care visits 38%. Black and Latino children had significant improvements. Black children saw 40% (ACT) and 66% (HCP) increases in well-controlled asthma, with reductions of 42% in ED and urgent care visits, 52% in acute care visits, and 49% and 67% declines in hospitalizations and PICU admissions, respectively. Latino children had 55% (ACT) and 33% (HCP) asthma control improvements, with 62%, 81%, and 50% drops in ED, urgent care, and acute care visits, respectively; hospitalizations decreased by 40% and PICU admissions by 100%.
The SBAT program would serve well as a model for enhancing controller medication adherence, reducing morbidity, and bridging the health disparities gap for children with poorly controlled asthma.
Reference:
Arcoleo K, McGovern C, Allen E, et al. School-based asthma therapy: Improving medication adherence, asthma control, and health care utilization. J. Allergy Clin. Immunol. 2025; 4(2): 100428. doi: 10.1016/j.jacig.2025.100428
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


