- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Surgical treatment better than CPAP in Sleep Apnea: JAMA
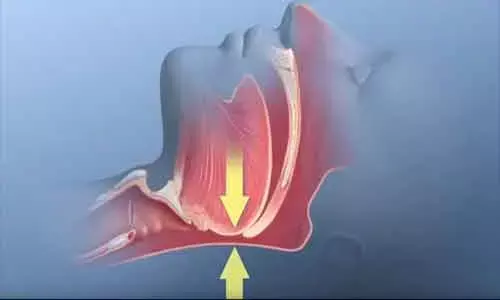
Stanford, California: Obstructive sleep apnea (OSA) patients treated surgically had a lower rate of systemic complications compared with those treated with CPAP, find a recent study. The findings of the study, published in the journal JAMA Otolaryngology - Head and Neck Surgery, suggest that surgery should constitute early treatment in patients at high risk of non adherence of CPAP or CPAP failure.
OSA is associated with cardiovascular, metabolic, psychiatric, and neurocognitive comorbidities as well as overall decreased survival. When considering only the Apnea Hypopnea Index as the treatment end point, the efficacy of surgical treatments for OSA is variable. However, only a few studies have shown an association between these procedures and improved clinically relevant outcomes such as cardiovascular, endocrine, and neurological sequelae of OSA. To fill this knowledge gap, Badr Ibrahim, Stanford University School of Medicine, Stanford Hospital and Clinics, Stanford, California, and colleagues evaluated the association of surgery for OSA with clinically relevant outcomes.
For the study, the researchers used the Truven MarketScan Database from January 1, 2007, to December 31, 2015 for identification of all patients diagnosed with OSA who received a prescription of continuous positive airway pressure (CPAP). The patients were aged from 40 to 89 years and had at least 3 years of data on file.
The researchers identified a total of 54 224 patients including a cohort of 49 823 patients who received CPAP prescription alone and 4269 patients who underwent soft tissue surgery. The median follow-up time was 4.47 years after the index CPAP prescription.
The occurrence of endocrine, neurological, and cardiovascular complications were compared in patients who received CPAP alone and those who received surgery.
Key findings of the study include:
- In the unadjusted model, soft tissue surgery was associated with decreased cardiovascular (hazard ratio [HR], 0.92), neurological (HR, 0.49), and endocrine (HR, 0.80) events.
- This finding was maintained in the adjusted model (HR for cardiovascular events, 0.91; HR for neurological events, 0.67; HR for endocrine events, 0.82.
- Skeletal surgery (n = 114) and concomitant skeletal and soft tissue surgery (n = 18) did not demonstrate significant differences in rates of development of systemic complications.
"In this cohort study, soft tissue surgery for OSA was associated with lower rates of development of neurological, cardiovascular, and endocrine systemic complications compared with CPAP prescription in a large convenience sample of the working insured US adult population," wrote the authors.
"These findings suggest that surgery should be part of the early treatment algorithm in patients at high risk of CPAP failure or nonadherence," they concluded.
The study titled, "Association of Systemic Diseases With Surgical Treatment for Obstructive Sleep Apnea Compared With Continuous Positive Airway Pressure," is published in the journal JAMA Otolaryngology - Head and Neck Surgery.
DOI: https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2775356
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


