- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Younger age and male sex linked to drug resistance to INH and rifampicin during treatment of TB
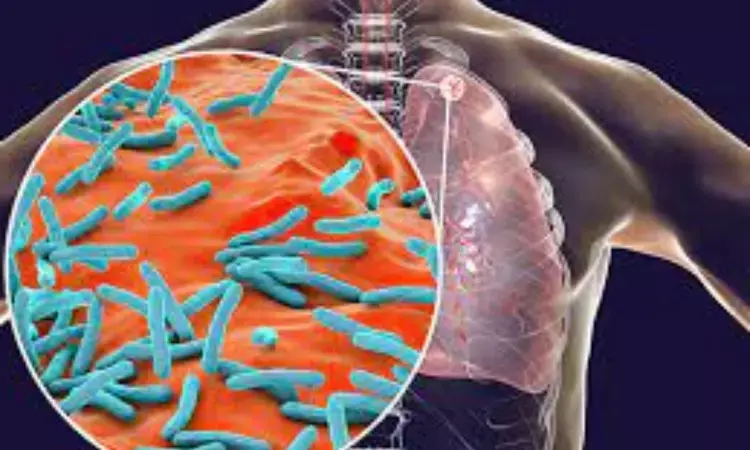
China: Males are at higher risks of drug resistance and Mycobacterium tuberculosis (MTB) infection, and younger age was tied to resistance isoniazid (INH) and rifampicin (RFP), MTB infection, and multidrug-resistant tuberculosis (MDR-TB), a recent study has revealed.
In their study, published in BMC Infectious Diseases, the researchers felt the need for further comprehensive monitoring of resistance patterns to control the MTB infection spread and local management of drug resistance.
Despite a long history of drug development, MTB infection remains a public health concern. Previous studies have reported a decrease in the incidence of MTB infection due to misdiagnosis and under-reporting; the actual number of cases could be far more significant. MDR-TB and RFP-resistant TB, notably, are particularly tenacious owing to the high mortality rate, the toxicity of anti-TB drugs, and the substantial economic burden.
Identification of the transmission mode and resistance mechanism of MTB is critical for the prevention of disease transmission. However, regional data are absent. Considering this, Zhenzhen Wang and a research team from China aimed to identify risk factors linked with MTB transmission, regional patterns of resistance to rifampicin and isoniazid, and the prevalence of MDR-TB.
For this purpose, the researchers conducted a high-resolution melt (HRM) analysis using pleural fluid samples, alveolar lavage fluid, and sputum collected from 17,515 participants with suspected or confirmed MTB infection in nine counties of Luoyang City and the downtown area from 2019 to 2021.
The study led to the following findings:
· Out of the 17,515 patients, 82.6% lived in rural areas, and 96.0% emerged for an initial screening.
· The HRM positivity rate was 16.8%, with a higher rate seen in males than females (18.0% vs. 14.1%).
· A positive sputum smear corresponds with a positive result for HRM analysis.
· The highest MTB infection rates by AgeAge occurred in males (22.9%) ages 26–30 years and females (28.1%) with AgeAge 21–25 years.
· RFP and INH resistance rates and the MDR incidence were higher in males than females (20.5% vs. 16.1%, 15.9% vs. 12.0%, and 12.9% vs. 10.2%).
· In previously treated patients, the HRM positivity rate was much higher than those newly diagnosed with MTB infection.
· Males at the initial screening had remarkably higher HRM favorable rates, INH resistance, RFP resistance, and MDR-TB than females, but not those previously treated for MTB infection.
· In the urban population, the drug resistance and HRM positivity rates were much higher versus the rural population.
· AgeAge < 51 years, previous treatment, male sex, and living in an urban area were remarkably and positively associated with drug resistance following adjustment for smear results and year of testing.
Isolation of the majority of resistant strains was done from males at the highest MTB infection risk in adulthood. Testing of this population, therefore, is essential. The highest rate of MTB infection was seen in females aged 21–25 and males aged 26–30.
"Prevention and control of MTB infection can not be taken lightly; urban populations, however, are also at high risk of high resistance rates and MTB infection," the researchers wrote. "Mutations to katG315 and codon 529–533 were tied to DR-TB and, thus, should be considered for selecting a treatment strategy."
To conclude, populations at high risk for MTB infection include males of all ages, females aged < 51 years, individuals previously treated for MTB infection, and those living in urban areas.
Reference:
Wang, Z., Guo, T., Jiang, T. et al. Regional distribution of Mycobacterium tuberculosis infection and resistance to rifampicin and isoniazid as determined by high-resolution melt analysis. BMC Infect Dis 22, 812 (2022). https://doi.org/10.1186/s12879-022-07792-7
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


