- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Intraoperative MRI successfully predicts newly diagnosed supratentorial glioblastoma: Study
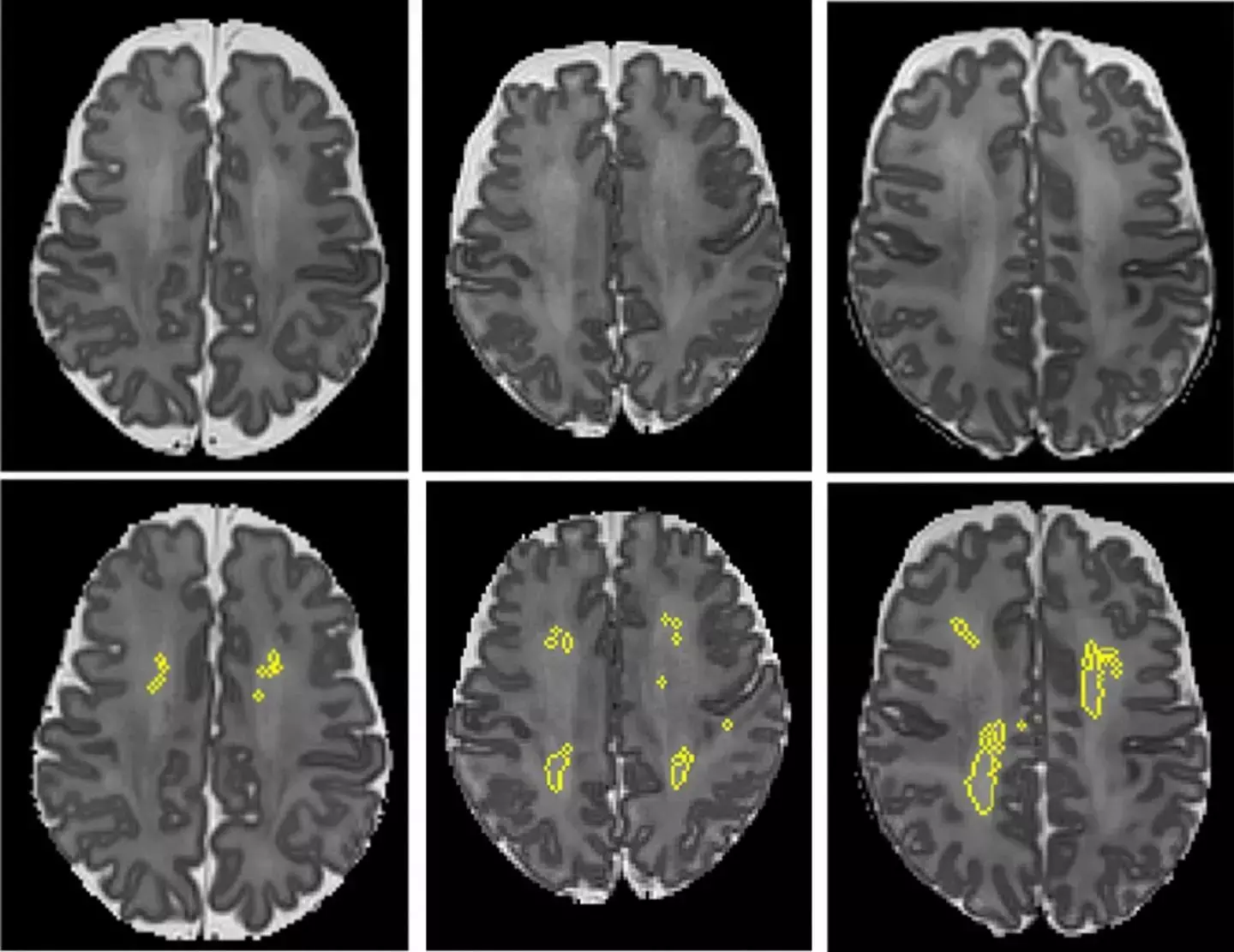
These MRI scans show diffuse white matter abnormality (DWMA). The top three panels display raw MRI images from very preterm infants born at 27 weeks (left), 26 weeks (center) and 31 weeks (right) gestation. Higher signal intensity can be seen in the central white matter, particularly for the 31-week gestation infant. The bottom panels display the corresponding slices with objectively segmented DWMA in yellow. The 27-week infant (left) was diagnosed with mild DWMA, the 26-week infant (center) was diagnosed with moderate DWMA, and the 31-week infant had severe DWMA.
CREDIT
Cincinnati Children's and Nature Scientific Reports
USAGE RESTRICTIONS
According to researchers from the Department of Neurosurgery, Washington University School of Medicine, St. Louis, Missouri, Gross-total resection (GTR) increased the overall survival rate for patients with newly diagnosed glioblastoma after adjusting for other prognostic factors and that iMRI increased EOR and GTR rate which was considered as a significant predictor of GTR.
This study is published in the Journal of Neurosurgery.
High-grade gliomas (HGGs) continue to carry poor prognoses, and patient outcomes depend heavily on the extent of resection (EOR). The utility of conventional image-guided surgery is limited by intraoperative brain shift. More recent techniques to maximize EOR, including intraoperative imaging and the use of fluorescent dyes, combat these limitations. However, the relative efficacy of these two techniques has never been systematically compared. There is rising evidence that in glioblastoma (GBM) surgery an increase of extent of resection (EoR) leads to an increase in patient survival. Intraoperative MRI (iMRI) is used in the surgical treatment of glioblastoma, with uncertain effects on outcomes.
Thus, Amar S Shah and colleagues carried out the present study to evaluate the impact of iMRI on the extent of resection (EOR) and overall survival (OS) while controlling for other known and suspected predictors.
They studied a total of 640 adult patients included in a multicenter retrospective cohort study. All patients were newly diagnosed with supratentorial glioblastoma who underwent resection. iMRI was performed in 332/640 cases (51.9%). Reviews of MRI features and tumor volumetric analysis were performed on a subsample of cases (n = 286; 110 non-iMRI, 176 iMRI) from a single institution.
Shah observed the following results from his study-
a. Gross-total resection (GTR) was achieved in 403/640 cases (63.0%).
b. Kaplan-Meier analysis of 286 cases with volumetric analysis for EOR showed longer OS for 100% EOR compared to all other groups.
c. Additional resection after iMRI was performed in 104/122 cases (85.2%) with an initial subtotal resection (STR), leading to a 6.3% mean increase in EOR and a 2.2-cm3 mean decrease in tumor volume.
d. For iMRI cases with volumetric analysis, the GTR rate increased from 54/176 (30.7%) on iMRI to 126/176 (71.5%) postoperatively.
e. The EOR was significantly higher in the iMRI group for intended GTR and STR groups.
f. Predictors of GTR on multivariate logistic regression included iMRI use and intended GTR.
g. Predictors of shorter OS on multivariate Cox regression included older age, STR, isocitrate dehydrogenase 1 (IDH1) wild type, no O6-methylguanine DNA methyltransferase (MGMT) methylation, and no Stupp therapy.
h. iMRI was a significant predictor of OS on univariate (HR 0.82, 95% CI 0.69-0.98; p = 0.03) but not multivariate analyses.
i. Use of iMRI was not associated with an increased rate of new permanent neurological deficits.
Therefore, they concluded that "GTR increased OS for patients with newly diagnosed glioblastoma after adjusting for other prognostic factors. iMRI increased EOR and GTR rate and was a significant predictor of GTR on multivariate analysis; however, iMRI was not an independent predictor of OS."
Additional supporting evidence is needed to determine the clinical benefit of iMRI in the management of glioblastoma, Shah further added.
For further reference, log in to:
Shah AS, Sylvester PT, Yahanda AT, Vellimana AK, Dunn GP, Evans J, Rich KM, Dowling JL, Leuthardt EC, Dacey RG, Kim AH, Grubb RL, Zipfel GJ, Oswood M, Jensen RL, Sutherland GR, Cahill DP, Abram SR, Honeycutt J, Shah M, Tao Y, Chicoine MR. Intraoperative MRI for newly diagnosed supratentorial glioblastoma: a multicenter-registry comparative study to conventional surgery. J Neurosurg. 2020 Oct 9:1-10. doi: 10.3171/2020.6.JNS19287. Epub ahead of print. PMID: 33035996.
Dr. Nandita Mohan is a practicing pediatric dentist with more than 5 years of clinical work experience. Along with this, she is equally interested in keeping herself up to date about the latest developments in the field of medicine and dentistry which is the driving force for her to be in association with Medical Dialogues. She also has her name attached with many publications; both national and international. She has pursued her BDS from Rajiv Gandhi University of Health Sciences, Bangalore and later went to enter her dream specialty (MDS) in the Department of Pedodontics and Preventive Dentistry from Pt. B.D. Sharma University of Health Sciences. Through all the years of experience, her core interest in learning something new has never stopped. She can be contacted at editorial@medicaldialogues.in. Contact no. 011-43720751
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


