- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Preoperative prostate MRI may predict urinary continence after prostatectomy: Study
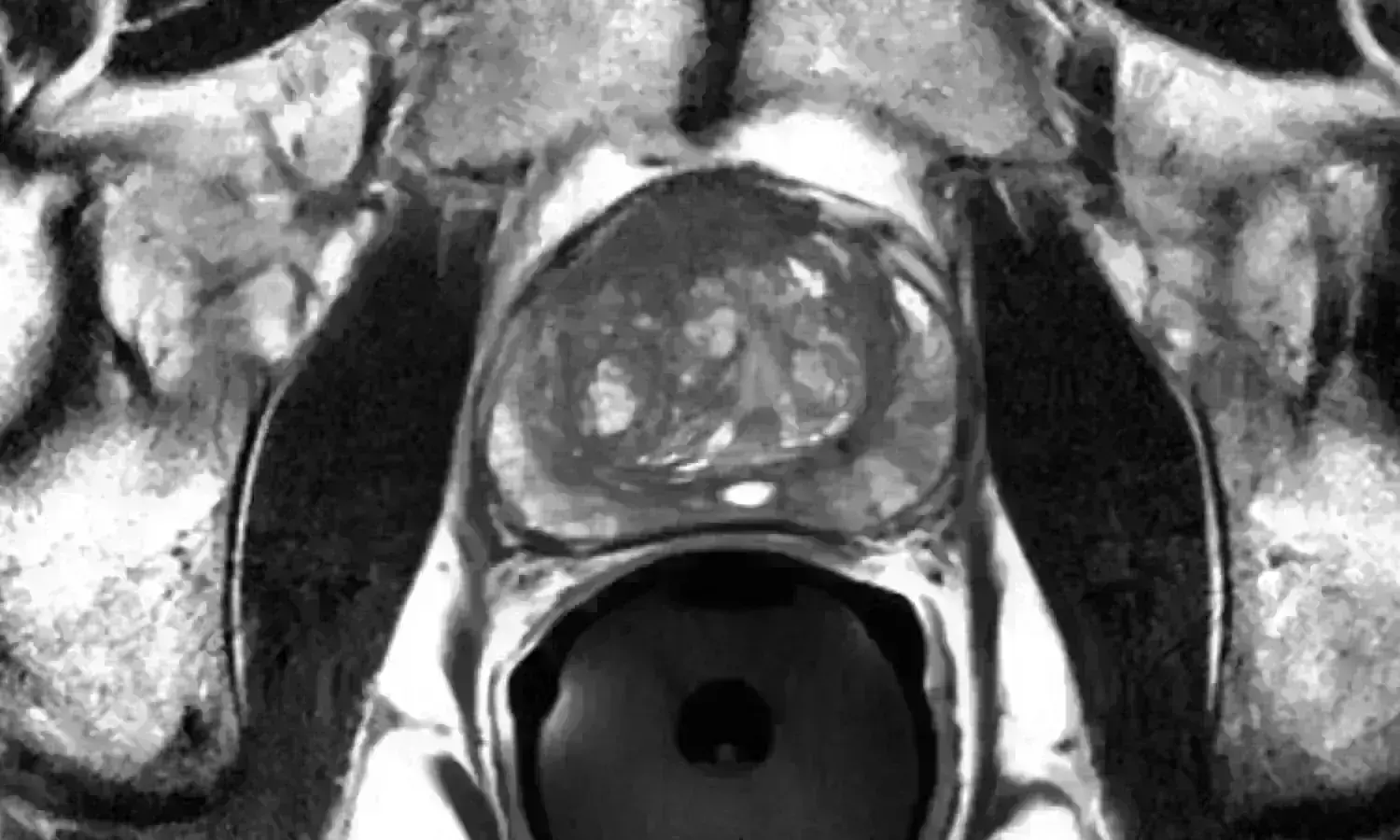
USA: Urethra length measured on MRI before surgery may predict urinary continence after prostatectomy, a recent study has found. The study was published in Radiology, the journal of the Radiological Society of North America, on Jan 18, 2022.
Urinary continence following radical prostatectomy (RP) is important in determining patients' quality of life. Anatomic measures at prostate MRI have been shown to be associated with continence outcomes. However, there is no clarity on their predictive ability and interrater agreement in comprehensive clinical models.
Against the above background, Hannah Lamberg, University of Michigan Medical School, Ann Arbor, Mich, and colleagues aimed to evaluate the predictive ability and interrater agreement of MRI-based anatomic measurements of post-RP continence when combined with clinical multivariable models in a retrospective cohort study.
For this purpose, the researchers evaluated continence outcomes in men who underwent RP from August 2015 to October 2019. These radiologists completed measure-specific training before participation. Logistic regression models were developed with clinical variables alone, MRI variables alone, and combined variables for predicting continence at 3, 6, and 12 months after RP; some patient data were missing at each time point. Using intraclass correlation coefficients (ICCs), interrater agreement of MRI variables was assessed.
A total of 586 men were included (mean age ± standard deviation: 63 years ± 7).
Following were the study's key findings:
- The proportion of patients with incontinence was 0.2% (one of 589) at baseline, 27% (145 of 529) at 3 months, 14% (63 of 465) at 6 months, and 9% (37 of 425) at 12 months.
- Longer coronal membranous urethra length (MUL) improved the odds of post-RP continence at all time points (odds ratio per 1 mm: 0.86; 0.86; and 0.79 respectively) in models that incorporated both clinical and MRI predictors. No other MRI variables were predictive.
- Age and baseline urinary function score were the only other predictive clinical variables at every time point. Interrater agreement was moderate (ICC, 0.62) for MUL among readers with measure-specific prostate MRI training and poor among those without the training (ICC, 0.38).
The researchers concluded, coronal membranous urethra length on preoperative prostate MRI scans was an independent predictor of post-prostatectomy continence; interrater agreement of this measure was higher after measure-specific training.
Reference:
The study titled, "Preoperative Prostate MRI Predictors of Urinary Continence Following Radical Prostatectomy," was published in the journal Radiology.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


