- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Rare case of Mesh Migration to neobladder following an incisional hernia
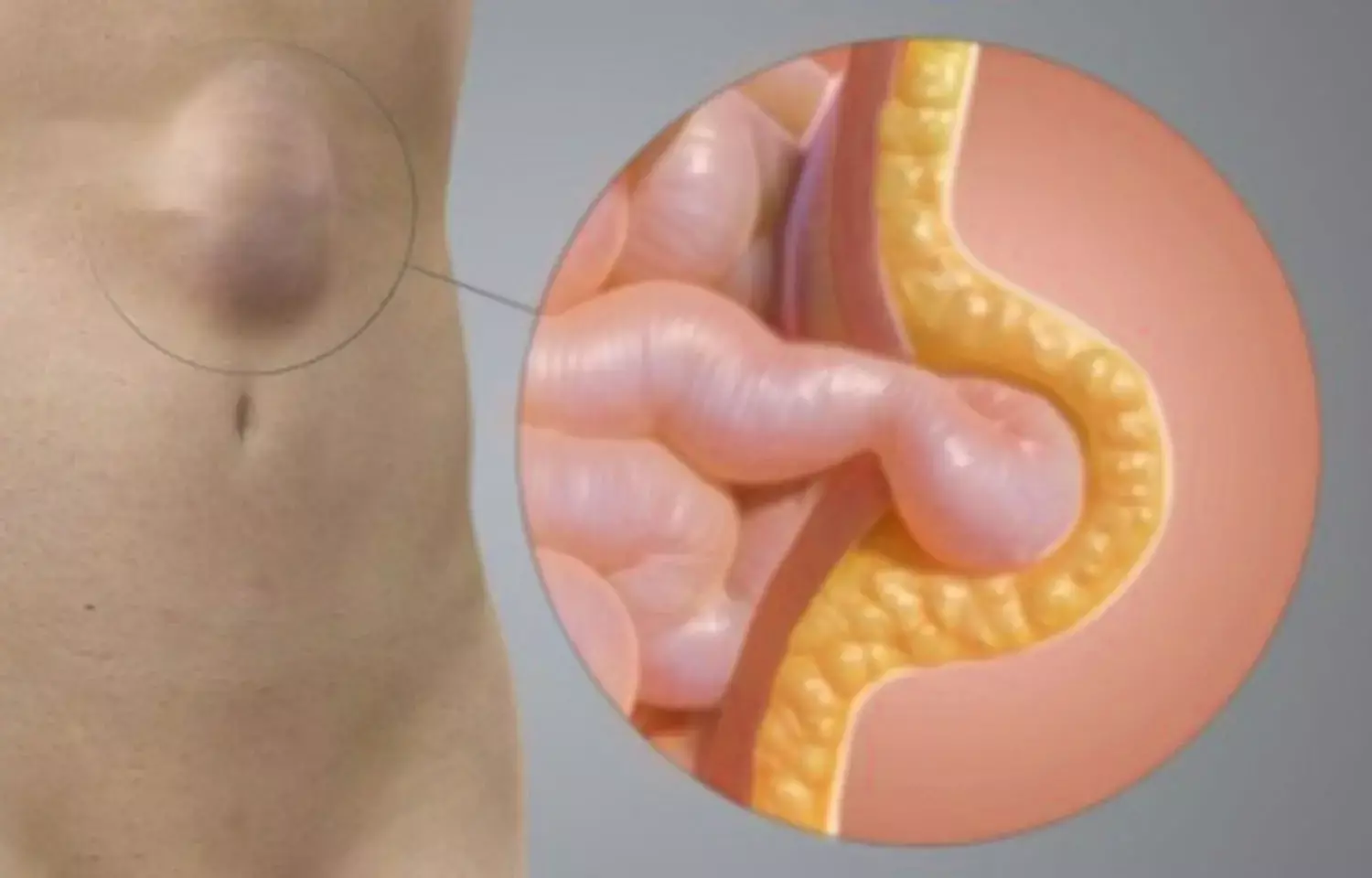
A recent case study describes a rare example of mesh migration into the neobladder and ileum, as well as complex fistula development after abdominal wall hernia surgery. Repair with no tension Mesh has become the usual treatment for incisional hernias in the abdominal wall. However, mesh infection, adhesions, and fistula development in other organs are documented as postoperative consequences. This case report was published in Hindawi.
Researchers have reported a case where an 80-year-old man underwent an incisional hernia repair utilizing a VentrioTM Hernia Patch with intraperitoneal insertion approach 3 years earlier and an open radical cystectomy with ileal neobladder reconstruction for bladder cancer 5 years prior. He had no additional medical history to speak of, nor did he have any family history to tell. He went to the hospital with a fever and stomach ache. A CT scan revealed that the mesh used to treat the abdominal wall hernia had moved into the neobladder and ileum. He was diagnosed with an entero-neobladder fistula caused by mesh migration, and conservative antibiotic therapy (TAZ/PIPC) was initiated.
The patient's health did not improve as a result of the conservative therapy, and he was sent to the current hospital one month later. A fistula was discovered on the lower abdomen's skin. Urine was also seen draining from the fistula. Urinalysis revealed occult blood and bacterial contamination, and urine culture revealed enteric bacteria. A hematological investigation indicated a normal white blood cell count of 8530/L, but C-reactive protein was high at 3.81 mg/dL. Cystography revealed the neobladder without the creation of a fistula, while cystoscopy revealed fecal debris and calcified mesh in the bladder. A CT scan of the abdomen revealed a migrating mesh into the neobladder and ileum. As a result, the patient was diagnosed with mesh migration into the neobladder and ileum, as well as entero-neobladder and entero-cutaneous fistulas caused by mesh infection.
As a corrective method the mesh was removed, and the neobladder and small intestine were partially resected. The mesh was strongly adhered to the neobladder and ileum, resulting in the creation of a fistula. The mesh was fully removed, and the neobladder and ileum were resected slightly. The neobladder wall defect was easily repaired, and the resected ileum was only approximately 20 cm long. The abdominal wall incisional hernia was treated with simple fascia suturing.
The patient complained of slight lower abdomen pain on the 13th postoperative day, and a transurethral (neobladder) cystography was conducted, suspecting leaking from the neobladder's closed location. It was also determined that there was no leaking. The CT scan on postoperative day 14 revealed subcutaneous fluid buildup in the belly. Drainage was necessary for 10 days, and antibiotics (PIPC) were provided, but the patient was released on postoperative day 40 without problems. Prior to surgery, the patient was nearly incontinent and required diapers. The patient was entirely incontinent after surgery, and blood tests revealed renal failure with a high serum creatinine level of 1.5. We opted to insert an indwelling urethral catheter postoperatively since he was unable to do intermittent catheter draining on his own.
In conclusion, when a hernia mesh is put in close proximity to a rebuilt organ, it is vital to remember that mesh displacement might cause injury to the reconstructed organ. To reduce organ damage from mesh displacement, the surgical approach should be designed to employ as little mesh as feasible. If mesh is utilized, the mesh type and technique of implantation and fixing should be chosen with greater care. Furthermore, if safe mesh repair was not achievable, autologous tissue repair techniques such as components separation procedure or free fascia grafting should have been used.
Reference:
Kuroiwa, M., Kitazawa, M., Miyagawa, Y., Muranaka, F., Tokumaru, S., Nakamura, S., Koyama, M., Yamamoto, Y., Hondo, N., Ehara, T., Miyazaki, S., Tanaka, H., & Soejima, Y. (2021). Mesh Migration into the Neobladder and Ileum with Complicated Fistula Formation following Incisional Hernia Repair. In E. Costantini (Ed.), Case Reports in Surgery (Vol. 2021, pp. 1–5). Hindawi Limited. https://doi.org/10.1155/2021/5683621
Medical Dialogues consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


