- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Intercostal Nerve Block Matches Epidural for Pain Relief in minimally invasive Lung Surgery: JAMA
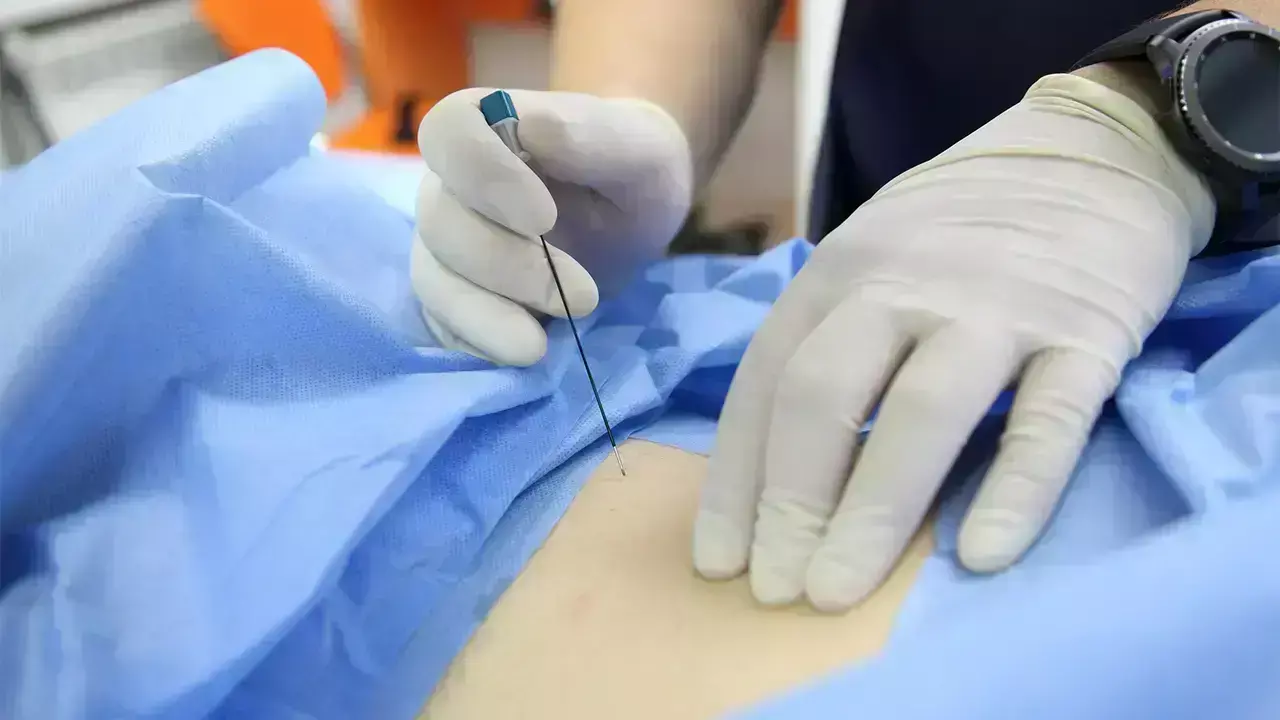
Researchers have found in OPtriAL randomized study that single-shot intercostal nerve block was noninferior to thoracic epidural analgesia for pain control in minimally invasive lung resections. In contrast, continuous paravertebral block was less effective than epidural. For patients at low risk of conversion to thoracotomy, intercostal nerve block is recommended as the preferred analgesic technique due to its less invasive nature and comparable efficacy.
Effective pain control after thoracic surgery is crucial for enhanced recovery. While thoracic epidural analgesia (TEA) traditionally ensures optimal analgesia, its adverse effects conflict with the principles of enhanced recovery after thoracic surgery. High-quality randomized data regarding less invasive alternative locoregional techniques are lacking. A study was done to evaluate the efficacy of continuous paravertebral block (PVB) and a single-shot intercostal nerve block (ICNB) as alternatives to TEA.
This randomized clinical trial compared PVB and ICNB vs TEA (1:1:1) in patients undergoing thoracoscopic anatomical lung resection at 11 hospitals in the Netherlands and Belgium, enrolled from March 5, 2021, to September 5, 2023. The study used a noninferiority design for pain and a superiority design for quality of recovery (QoR). Primary outcomes were pain, defined as mean proportion of pain scores 4 or greater during postoperative days (POD) 0 through 2 (noninferiority margin for the upper limit [UL] 1-sided 98.65% CI, 17.5%), and QoR, assessed with the QoR-15 questionnaire at POD 1 and 2.
Secondary measures included opioid consumption, mobilization, complications, and hospitalization. Results A total of 450 patients were randomized, with 389 included in the intention-to-treat (ITT) analysis (mean [SD] age, 66 [9] years; 208 female patients [54%] and 181 male [46%]). Of these 389 patients, 131 received TEA, 134 received PVB, and 124 received ICNB.
The mean proportions of pain scores 4 or greater were 20.7% (95% CI, 16.5%-24.9%) for TEA, 35.5% (95% CI, 30.1%-40.8%) for PVB, and 29.5% (95% CI, 24.6%-34.4%) for ICNB. While PVB was inferior to TEA regarding pain (ITT: UL, 22.4%; analysis per-protocol [PP]: UL, 23.1%), ICNB was noninferior to TEA (ITT: UL, 16.1%; PP: UL, 17.0%). The mean (SD) QoR-15 scores were similar across groups: 104.96 (20.47) for TEA, 106.06 (17.94; P = .641) for PVB (P = .64 for that comparison), and 106.85 (21.11) for ICNB (P = .47 for that comparison). Both ICNB and PVB significantly reduced opioid consumption and enhanced mobility compared with TEA, with no significant differences in complications. Hospitalization was shorter in the ICNB group. After thoracoscopic anatomical lung resection, only ICNB provides noninferior pain relief compared with TEA. ICNB emerges as an alternative to TEA, although risks and benefits should be weighed for optimal personalized pain control.
Reference:
Spaans LN, Dijkgraaf MGW, Susa D, et al. Intercostal or Paravertebral Block vs Thoracic Epidural in Lung Surgery: A Randomized Noninferiority Trial. JAMA Surg. Published online June 25, 2025. doi:10.1001/jamasurg.2025.1899
=
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


