- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Intra-operative measurements of testicular vasal lumen diameter can be an adjunctive factor that may influence choice of VR technique: Study
Researchers have found in a new study that Intra-operative measurements of the testicular vasal lumen diameter may serve as an adjunctive factor in determining the appropriate vasectomy reversal (VR) technique. This information can aid in pre-operative counseling and potentially improve VR success rates.
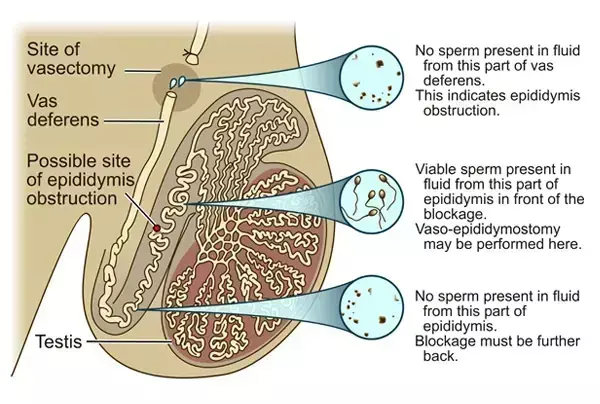
Vasectomy reversal (VR) can be a challenging surgery and numerous factors have been identified to guide surgical decision-making to optimize success. The objective of this study was to identify pre-operative and intra-operative factors associated with VR surgical method and success. Additionally, we aimed to investigate the role of testicular vas deferens diameter in surgical decision-making and success.
This study was a retrospective cohort of men >18 years of age who underwent a VR at our Institution from January 2008 to June 2023. Qualified patients underwent chart review and details recorded included age, obstructive interval, surgical technique, vasal lumen diameters, presence of sperm granuloma or surgical clips, sperm quality, and vasal fluid quality. Semen analysis (SA) parameters were also recorded. Pregnancy outcomes were ascertained via telephone interview.
Descriptive statistics and correlations were analyzed with two-sample t-tests for continuous and chi-square or Fisher's exact tests for categorical characteristics. Logistic regression using generalized estimating equation (GEE) methods was used to estimate associations of diameter with surgery types unadjusted and adjusted for patient and intra-operative fluid characteristics. Results: A total of 710 patients underwent VR during the study period and 326 post-operative semen analyses were available for review.
Average patient was 38 years old, with an obstructive interval of 10 years. Vasoepididymostomy (VE) had modestly larger observed mean testicular vasal lumen diameter (0.94 mm) versus vasovasostomy (VV; 0.88 mm; p = 0.10). However, diameter ≥1 mm was associated with >2 times higher odds of VE versus VV (odds ratio [OR] 2.12; p < 0.01) adjusted for several patient characteristics. VE was associated with lower frequency of positive post-operative semen analyses (64.4% VV/VE or bilateral VE vs. 92.4% bilateral VV), and longer obstructive interval (11.5 years VV/VE or bilateral VE vs. 7.84 years bilateral VV).
There were higher rates of spermatozoa on post-operative SAs when bilateral VV was performed (VV/VV 92.3%; VV/VE 73.3%; VE/VE 51.5%; p < 0.001). Of the 207 patients with pregnancy data, 103 (49.8%) experienced pregnancy following VR. Intra-operative measurements of testicular vasal lumen diameter can be an adjunctive factor that may influence choice of VR technique. This finding can help guide pre-operative surgical counseling and VR success rates.
Reference:
Maloney TJ, Armstrong DB, Grant LJ, Bowling GC, Zamani M, Watson N, Dean RC, Hawksworth DJ. Testicular vasal diameter: A new intra-operative predictor of vasectomy reversal success? Andrology. 2025 Jul 11. doi: 10.1111/andr.70098. Epub ahead of print. PMID: 40643103.
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


