- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
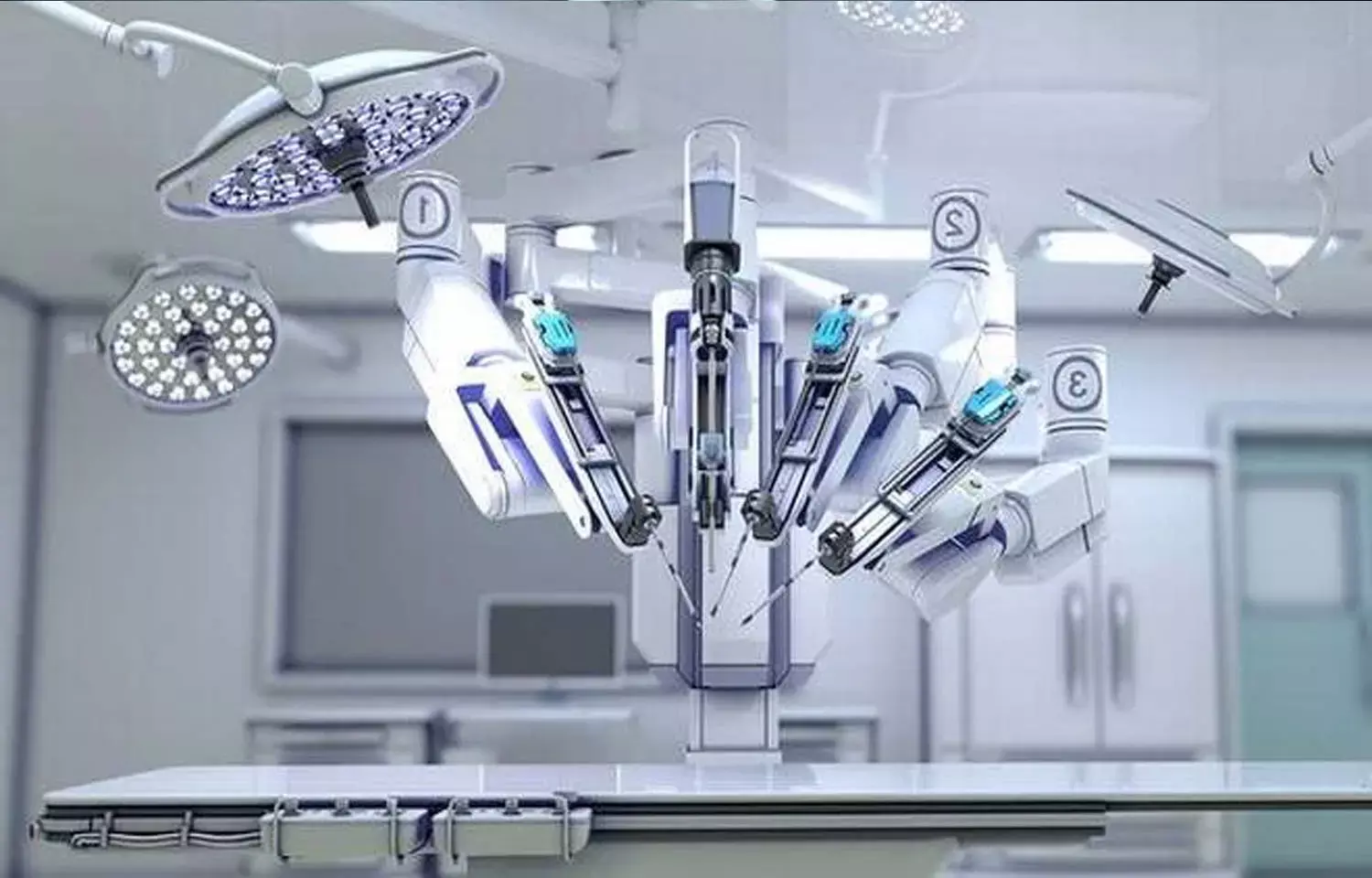
Is robot-assisted radical cystectomy better for patient recovery than open surgery?
USA: In a new study conducted by Vivek Venkatramani and team, it was found that after radical cystectomy, patients take 3 to 6 months to return to baseline levels, regardless of surgical method. The findings of this study were published in the Journal of American Medical Association.
After radical cystectomy, no data on time to recovery of patient-reported and performance-related markers of functional independence available (open or robotic). As a result, the goal of this study was to see if functional independence could be restored following radical cystectomy and if robot-assisted radical cystectomy (RARC) has any advantages over open procedures.
The RAZOR (Randomized Open vs Robotic Cystectomy) experiment provided the data for this secondary analysis. RAZOR was a phase 3 multicenter noninferiority study that ran from July 1, 2011, to November 18, 2014, at 15 academic medical institutions across the United States, with a median follow-up of two years. The per-protocol population (n = 302) was among the participants.
From February 1, 2017, through May 1, 2021, data was evaluated. The subjects had robotic-assisted radical cystectomy (RARC) or open radical cystectomy (ORC). The measures of independence were patient-reported (activities of daily living [ADL] and independent ADL [iADL]) and performance-related (handgrip strength [HGS] and Timed Up & Go walking test [TUGWT]). Postoperative recovery Patterns for the entire cohort were studied, as well as comparisons between RARC and ORC. Exploratory analyses were conducted to evaluate measures of independence among diversion types and to see if baseline deficits were linked to 90-day complications or 1-year mortality.
The key findings are as follow:
1. 150 of the 302 patients in the study received RARC, while 152 underwent ORC.
2. Both groups had identical baseline characteristics. ADL, iADL, and TUGWT returned to baseline in the whole sample after three months, but HGS took six months.
3. At any point in time, there was no difference in ADL, iADL, TUGWT, or HGS scores between RARC and ORC. RARC took one month to restore activities of daily life, but ORC took three months to recover.
4. After RARC, handgrip strength returned in 3 months vs. 6 months after ORC. At 3 months, 32 of 90 patients (35.6%) in the RARC group demonstrated recovery in HGS vs 32 of 88 (36.4 percent) in the ORC group, suggesting that the major research hypothesis was rejected.
5. Patients who had a continent urine diversion recovered faster than those who had a noncontinent urinary diversion, with no differences in other parameters. There was no link between baseline deficits in any measure and 90-day complications or 1-year mortality.
In conclusion, these data will be extremely useful in patient counseling and planning. When compared to ORC, handgrip strength and ADL returned to baseline sooner following RARC; however, there was no difference in the percentage of patients who recovered. Further study is needed to assess the clinical significance of these findings.
Reference:
Venkatramani V, Reis IM, Gonzalgo ML, et al. Comparison of Robot-Assisted and Open Radical Cystectomy in Recovery of Patient-Reported and Performance-Related Measures of Independence: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open. 2022;5(2):e2148329. doi:10.1001/jamanetworkopen.2021.48329
Medical Dialogues consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


