- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Mechanochemical ablation and cyanoacrylate adhesive have similar pain scores during truncal vein reflux treatment
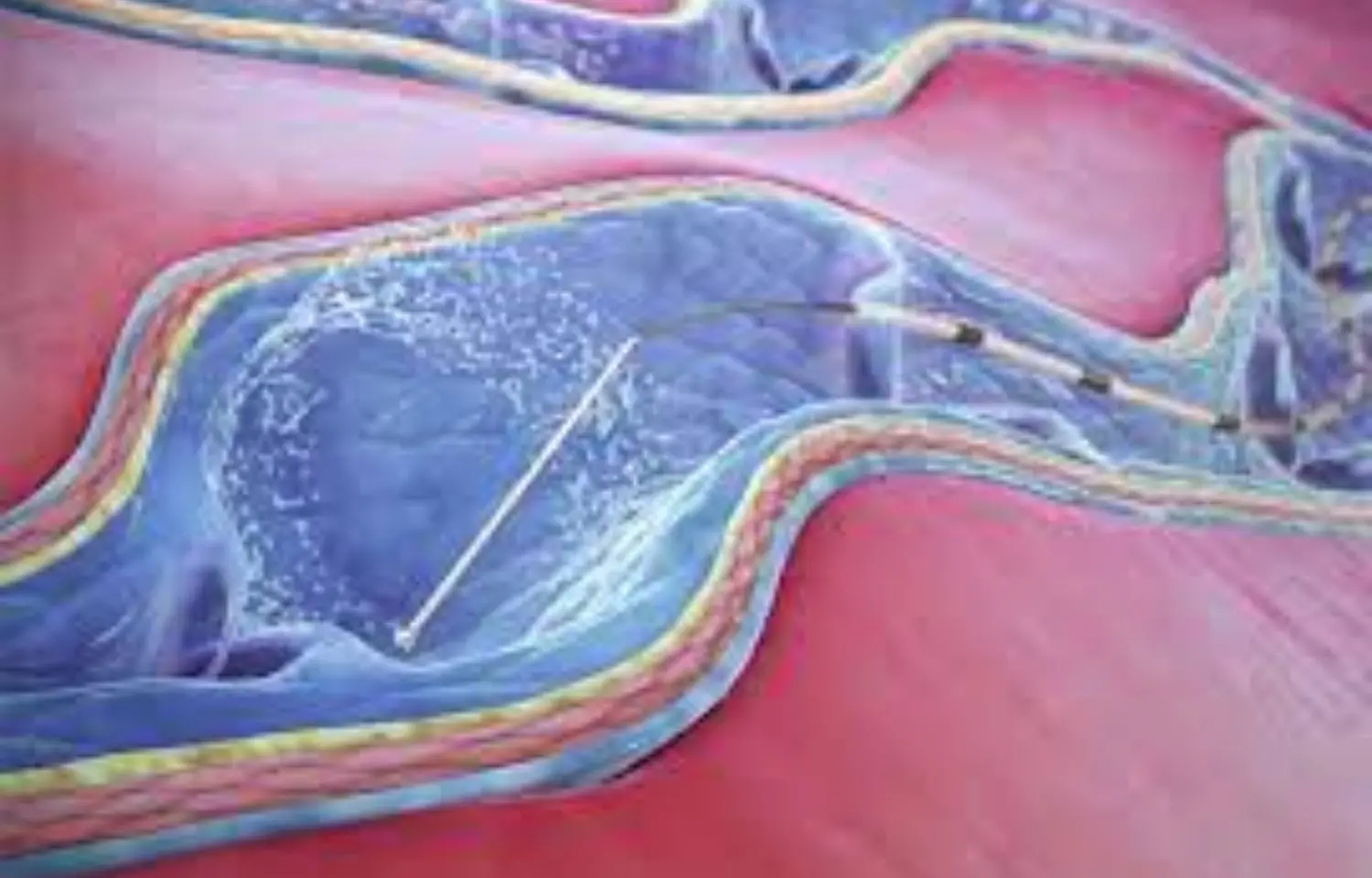
UK: New research directly comparing nontumescent ablation techniques found both the techniques -- mechanochemical ablation (MOCA) and cyanoacrylate adhesive injection (CAE) -- have similar periprocedural pain scores. This suggests that determining which interventions to use can be based on clinician and patient preference and cost-effectiveness. The study appears in the journal JAMA Surgery.
Recommended first-line treatment for truncal vein reflux is endovenous thermal ablations (ETAs), having a short recovery time and are cost-effective. However, ETAs can lead to discomfort during tumescent anesthesia infiltration. nontumescent ablation techniques had emerged in the form of MOCA and CAE to minimize discomfort, nonthermal.
Amjad Belramman, Imperial College London, London, United Kingdom, and colleagues aimed to assess pain scores immediately after truncal ablation using a 100-mm visual analog scale and 10-point number scale to compare pain-related outcomes following mechanochemical ablation vs cyanoacrylate adhesive treatment in the Multicenter Randomized II Clinical Trial Comparing Mechanochemical Ablation vs Cyanoacrylate Adhesive for the Treatment of Primary Truncal Saphenous Veins Incompetence study.
The study was a prospective multicenter randomized clinical trial conducted at 3 sites between November 2017 and January 2020. Patients with primary great or small saphenous varicose veins were included and those with recurrent varicose veins, current deep venous thrombosis, or serious arterial disease were excluded. Out of 392 screened participants, 225 were excluded, and 167 participants underwent randomization. 4 participants did not get allocated intervention and were included in the intention-to-treat analysis. They were followed at 2 weeks, and 3, 6, and 12 months.
Patients with primary truncal vein incompetence were randomized to receive either MOCA or CAE. Pain score immediately after completing truncal ablation using a 100-mm visual analog scale (VAS) and a 10-point number scale was the primary outcome.
Of 167 study participants, 99 (59.3%) were women, and the mean age was 56 years. Overall, 155 truncal veins treated (92.8%) were great saphenous veins.
The study revealed the following findings:
- Demographic data and baseline status were comparable between treatment groups. A total of 73 patients (47%) underwent adjunctive treatment of varicosities.
- Overall median maximum pain score after truncal treatment was 23 mm on the VAS and 3 on the number scale, showing no significant difference in median (IQR) pain measured by VAS (MOCA, 24 mm vs CAE, 20 mm) or by number scale (MOCA, 4 vs CAE, 3).
- Both groups demonstrated significant and comparable improvement in clinical severity, generic and disease-specific QoL scores, and complete occlusion rates.
- Four patients treated with CAE developed minor complications (superficial thrombophlebitis and thrombus extensions).
"To our knowledge, this was the first randomized clinical trial directly comparing nontumescent ablation techniques," wrote the authors. "Both nontumescent ablation techniques had comparable outcomes, suggesting that determining which interventions to use can be based on cost-effectiveness and clinician and patient preference."
Reference:
Henke P. Relevant Outcomes in Superficial Venous Ablation Treatments. JAMA Surg. Published online April 06, 2022. doi:10.1001/jamasurg.2022.0299
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


