- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Sacrocolpopexy superior to native tissue repair for surgical repair of vaginal vault prolapse after hysterectomy: JAMA
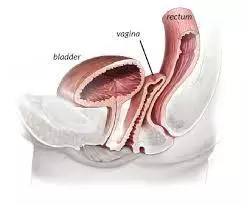
Sacrocolpopexy superior to native tissue repair for surgical repair of vaginal vault prolapse after hysterectomy suggests a new study published in the JAMA.
The optimal surgical repair of vaginal vault prolapse after hysterectomy remains undetermined. A study was done to compare the efficacy and safety of 3 surgical approaches for vaginal vault prolapse after hysterectomy. This was a multisite, 3-arm, superiority and noninferiority randomized clinical trial. Outcomes were assessed biannually up to 60 months, until the last participant reached 36 months of follow-up. Settings included 9 clinical sites in the US National Institute of Child Health and Human Development (NICHD) Pelvic Floor Disorders Network. Between February 2016 and April 2019, women with symptomatic vaginal vault prolapse after hysterectomy who desired surgical correction were randomized. Data were analyzed from November 2022 to January 2023.
The primary outcome was time until composite treatment failure (including retreatment for prolapse, prolapse beyond the hymen, or prolapse symptoms) evaluated with survival models. Secondary outcomes included patient-reported symptom-specific results, objective measures, and adverse events. Results : Of 376 randomized participants (mean [SD] age, 66.1 [8.7] years), 360 (96%) had surgery, and 296 (82%) completed follow-up. Adjusted 36-month failure incidence was 28% (95% CI, 20%-37%) for sacrocolpopexy, 29% (95% CI, 21%-38%) for transvaginal mesh, and 43% (95% CI, 35%-53%) for native tissue repair. Sacrocolpopexy was found to be superior to native tissue repair (adjusted hazard ratio [aHR], 0.57; 99% CI, 0.33-0.98; P = .01).
Transvaginal mesh was not statistically superior to native tissue after adjustment for multiple comparisons (aHR, 0.60; 99% CI, 0.34-1.03; P = .02) but was noninferior to sacrocolpopexy (aHR, 1.05; 97% CI, 0-1.65; P = .01). All 3 surgeries resulted in sustained benefits in subjective outcomes. Mesh exposure rates were low (4 of 120 [3%] for sacrocolpopexy and 6 of 115 [5%] for transvaginal mesh) as were the rates of dyspareunia. Among participants undergoing apical repair for vaginal vault prolapse, sacrocolpopexy and transvaginal mesh resulted in similar composite failure rates at study completion; both had lower failure rates than native tissue repair, although only sacrocolpopexy met a statistically significant difference. Low rates of mesh complications and adverse events corroborated the overall safety of each approach.
Reference:
Menefee SA, Richter HE, Myers D, et al. Apical Suspension Repair for Vaginal Vault Prolapse: A Randomized Clinical Trial. JAMA Surg. Published online May 22, 2024. doi:10.1001/jamasurg.2024.1206
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


