- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Hyperbaric Ropivacaine useful alternative to bupivacaine for spinal anesthesia with better motor recovery profiles: Study
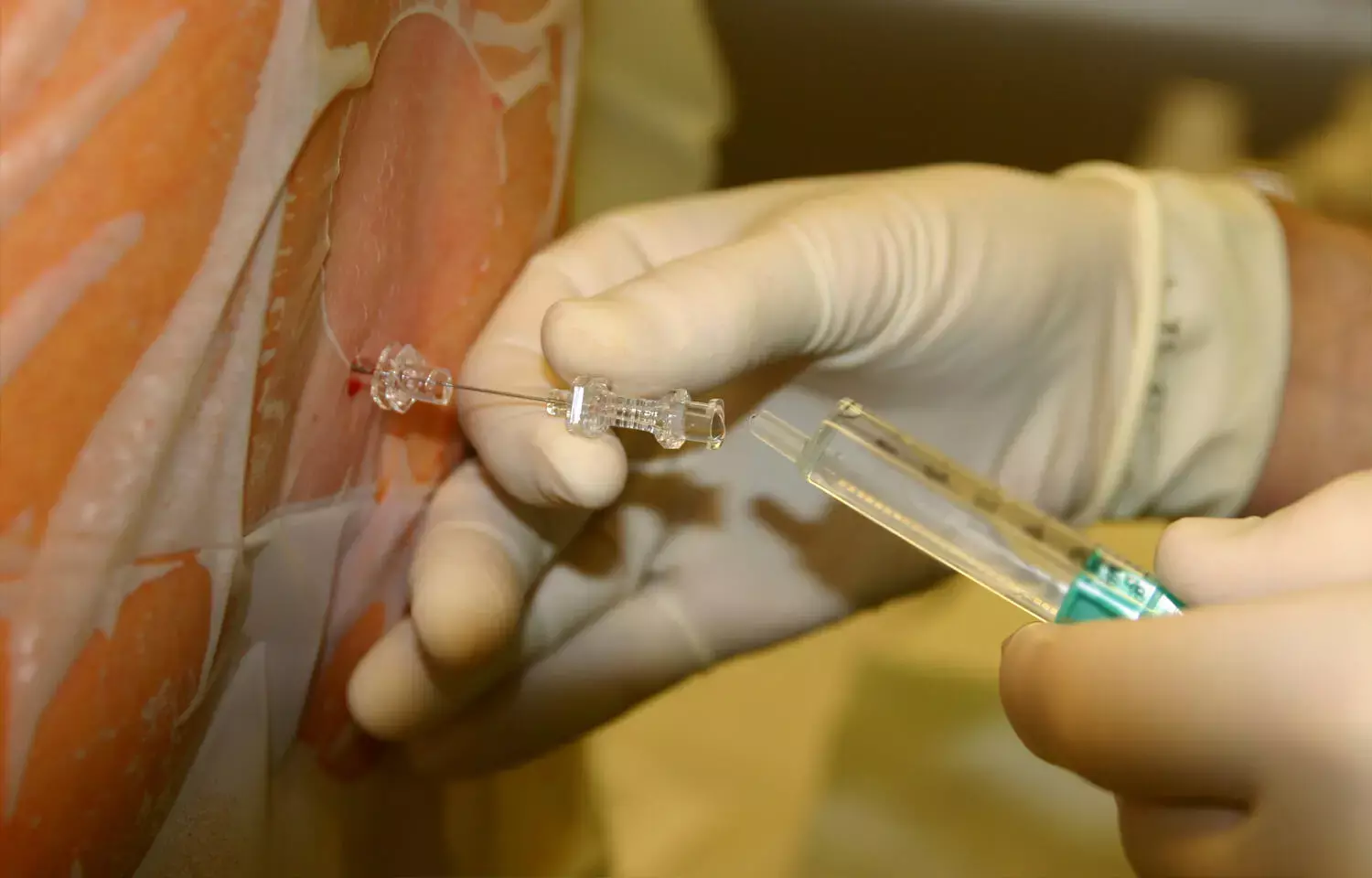
Recently published study investigated the efficacy and safety of hyperbaric 0.75% ropivacaine compared to 0.5% bupivacaine in spinal anesthesia for patients undergoing infra-umbilical surgeries. The double-blind, randomized, active-controlled, parallel arm study involved 60 patients and focused on parameters like onset and duration of sensory and motor block, time to rescue analgesia, hemodynamics, and safety. Results indicated a slower onset but faster regression of sensory and motor blockades with ropivacaine compared to bupivacaine. However, the duration of sensory blockade and requirement for rescue analgesia were comparable between the two drugs. Ropivacaine also caused fewer side effects. The study highlighted that the equipotent dose of 0.75% ropivacaine proved to be a comparable and safer alternative to 0.5% bupivacaine, with better motor recovery profiles. However, it suggested caution for time-sensitive cases due to the slower onset of ropivacaine.
The study employed a computer-generated random number table for patient allocation into groups, ensuring the double-blinding of participants and proper ethical considerations. The physical characteristics of the two groups were comparable, and the study found delayed sensory and motor block onset with ropivacaine, but a comparable total duration of sensory blockade and time required for rescue analgesia. Hemodynamic changes, incidence of bradycardia, nausea, vomiting, and shivering did not significantly differ between the two groups. The study concluded that 0.75% hyperbaric ropivacaine demonstrated clinically effective anesthesia and suggested its potential as an efficient and safe alternative to the commonly used bupivacaine in routine clinical practice.
It provided valuable insights into the use of hyperbaric ropivacaine and its comparable efficacy and safety with bupivacaine in the context of spinal anesthesia for infra-umbilical surgeries. The study's strengths included randomization and an adequate sample size, but it also acknowledged limitations such as focusing on relatively healthy adults and elective surgeries. Nonetheless, it shed light on the potential of hyperbaric ropivacaine as an alternative to bupivacaine in clinical practice, emphasizing its potential benefits and highlighting areas for further consideration and research.
Key Points
- The study compared the efficacy and safety of hyperbaric 0.75% ropivacaine to 0.5% bupivacaine in spinal anesthesia for infra-umbilical surgeries in a double-blind, randomized, active-controlled, parallel arm study involving 60 patients. It focused on parameters like onset and duration of sensory and motor block, time to rescue analgesia, hemodynamics, and safety.
- The study revealed valuable insights into the use of hyperbaric ropivacaine as a comparable and safer alternative to bupivacaine in the context of spinal anesthesia for infra-umbilical surgeries. It employed randomization and an adequate sample size but acknowledged limitations, emphasizing its potential benefits and highlighting areas for further consideration and research.
Reference –
Kalbande J V, Kukanti C, Karim H R, et al. (March 26, 2024) The Efficacy and Safety of Spinal Anesthesia With Hyperbaric Ropivacaine 0.75% and Bupivacaine 0.5% in Patients Undergoing Infra-Umbilical Surgeries: A Randomized, Double-Blind Study. Cureus 16(3): e57005. DOI 10.7759/cureus.57005
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


