- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Is antibiotic prophylaxis necessary for patients undergoing extracorporeal membrane oxygenation?
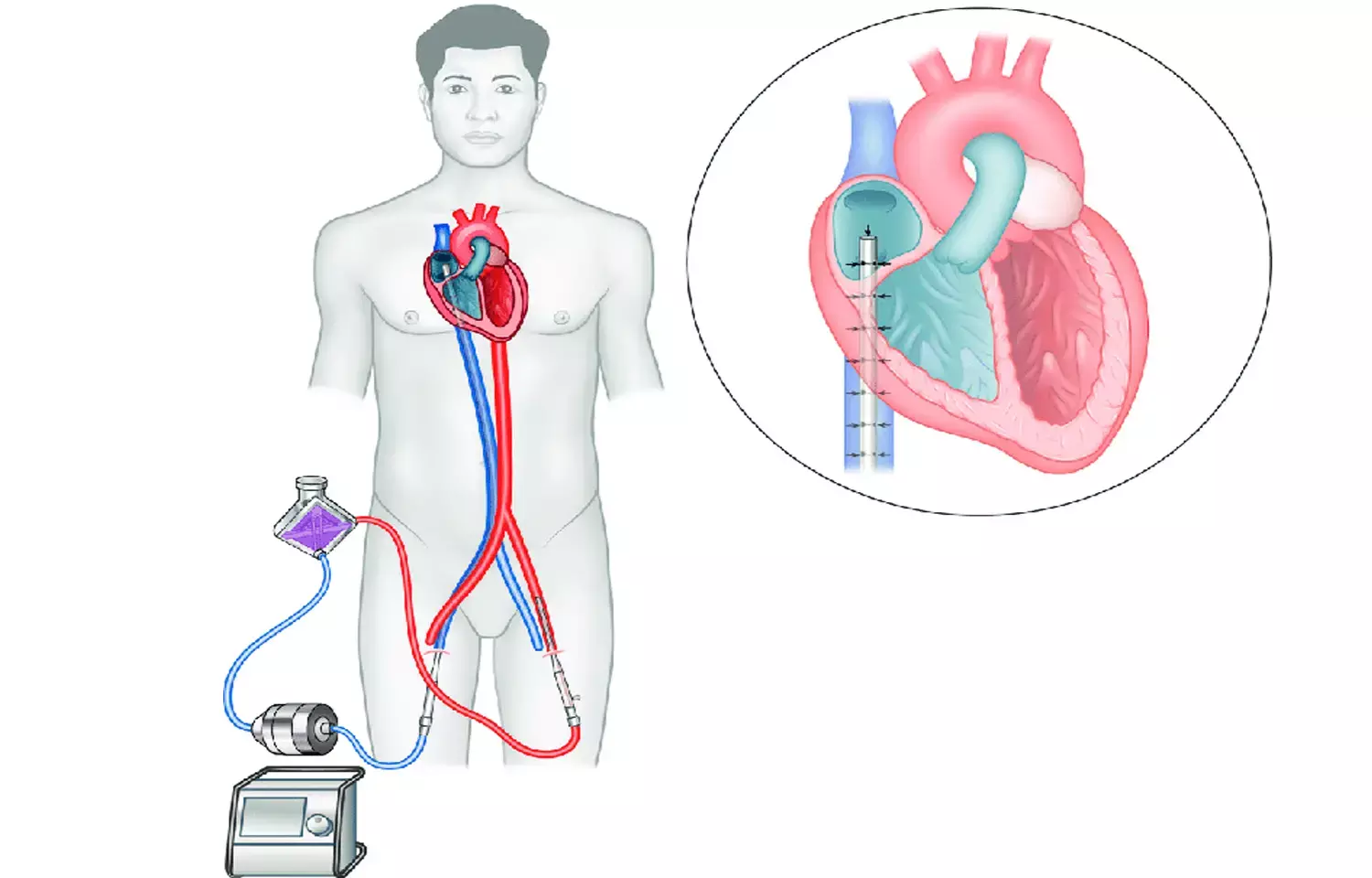
In recent times, the utilization of Extracorporeal Membrane Oxygenation (ECMO) has increased. By employing ECMO in the ICU, the care for adult and pediatric patients suffering from acute respiratory or cardiac failure can be enhanced. Recent research study examined the use of antibiotic prophylaxis for patients undergoing Extracorporeal Membrane Oxygenation (ECMO). ECMO patients are highly susceptible to infections, with high rates of sepsis and nosocomial infections. The study objectives were to investigate whether antibiotic prophylaxis can decrease 30-day mortality and prevent the occurrence of nosocomial infections in ECMO patients. A systematic review and meta-analysis were conducted, including 5 retrospective studies with a pooled population of 7,996 patients.
Results on Mortality and Infections
Regarding 30-day mortality, the random-effects model found no statistically significant difference between the antibiotic prophylaxis group and the non-prophylaxis group (OR 0.76; 95%CI 0.37–1.59). For the rate of nosocomial infections, the fixed-effect model showed an OR of 0.81 (95%CI 0.71–0.92) in favor of the antibiotic prophylaxis group, with a number-needed-to-treat of 39.7 patients.
Quality of Evidence
The quality of evidence for both outcomes was assessed as very low, indicating high risks of bias, inconsistency, and potential confounding factors. The retrospective nature of the studies and small sample sizes limit the reliability of the conclusions.
The study findings suggest that antibiotic prophylaxis may have no significant impact on reducing 30-day mortality in ECMO patients, but may decrease the incidence of nosocomial infections, albeit with a high number needed to treat. However, these results are provisional due to the low quality of available evidence.
Recommendations for Future Research
The authors recommend conducting high-quality prospective studies, including randomized controlled trials, to further investigate the specific clinical questions regarding the use of antibiotic prophylaxis in ECMO patients. More research is needed to determine the optimal antibiotic regimen, duration of prophylaxis, and the potential impact on different ECMO patient populations and infection outcomes.
Key Points
1. The study examined the use of antibiotic prophylaxis for patients undergoing Extracorporeal Membrane Oxygenation (ECMO), as ECMO patients are highly susceptible to infections with high rates of sepsis and nosocomial infections.
2. The study objectives were to investigate whether antibiotic prophylaxis can decrease 30-day mortality and prevent the occurrence of nosocomial infections in ECMO patients. A systematic review and meta-analysis were conducted, including 5 retrospective studies with a pooled population of 7,996 patients.
3. Regarding 30-day mortality, the random-effects model found no statistically significant difference between the antibiotic prophylaxis group and the non-prophylaxis group. For the rate of nosocomial infections, the fixed-effect model showed a lower rate in the antibiotic prophylaxis group, with a number-needed-to-treat of 39.7 patients.
4. The quality of evidence for both outcomes was assessed as very low, indicating high risks of bias, inconsistency, and potential confounding factors. The retrospective nature of the studies and small sample sizes limit the reliability of the conclusions.
5. The study findings suggest that antibiotic prophylaxis may have no significant impact on reducing 30-day mortality in ECMO patients, but may decrease the incidence of nosocomial infections, albeit with a high number needed to treat. However, these results are provisional due to the low quality of available evidence.
6. The authors recommend conducting high-quality prospective studies, including randomized controlled trials, to further investigate the specific clinical questions regarding the use of antibiotic prophylaxis in ECMO patients. More research is needed to determine the optimal antibiotic regimen, duration of prophylaxis, and the potential impact on different ECMO patient populations and infection outcomes.
Reference –
Orso D, Fodale CM, Fossati S, Venturini S, Fonda F, Cugini F, Comisso I, Crapis M, Cacciavillani L, Bove T. Do patients receiving extracorporeal membrane-oxygenation need antibiotic prophylaxis? A systematic review and meta-analysis on 7,996 patients. BMC Anesthesiol. 2024 Nov 12;24(1):410. doi: 10.1186/s12871-024-02796-z. PMID: 39533181; PMCID: PMC11556216.
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


