- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Optimizing Anesthetic Techniques for Percutaneous Kyphoplasty: A Comparative Study of TPVB and Local Infiltration
Recent randomized controlled trial compared the efficacy and safety of thoracic paravertebral nerve block (TPVB) versus local infiltration (LI) anesthesia during percutaneous kyphoplasty (PKP) in patients with thoracic osteoporotic vertebral compression fractures (OVCFs) combined with intercostal neuralgia (IN). The study enrolled 60 patients aged over 60 with single-level T8-T12 thoracic compression fractures accompanied by significant thoracic and intercostal pain. Patients were randomly assigned to receive either TPVB or LI anesthesia during PKP.
Methodology
• Anesthesia Techniques:
• TPVB: Ultrasound-guided injection of 10 mL of 0.5% ropivacaine into the thoracic paravertebral space targeting multiple nerve branches and the sympathetic trunk.
• LI: Injection of 5 mL of 1% lidocaine and 10 mL of 0.5% ropivacaine locally around the puncture site.
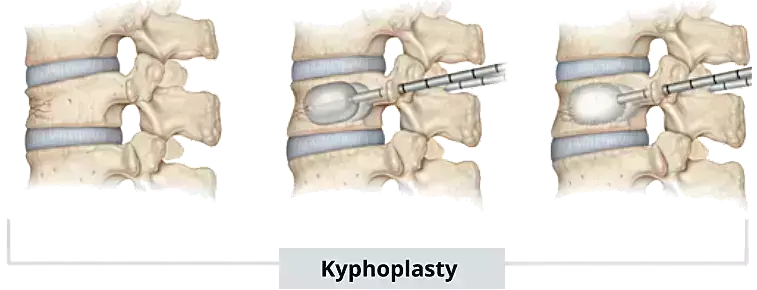
• PKP Procedure: Standard unilateral percutaneous kyphoplasty was performed with balloon inflation and polymethyl methacrylate (PMMA) cement injection under fluoroscopic guidance.
• Outcome Measures: Primary outcomes included visual analog scale (VAS) scores during the procedure and postoperatively. Secondary outcomes were anesthesia satisfaction (PAS), SF-36 quality of life scores, Oswestry Disability Index (ODI), intraoperative hemodynamics (MAP and HR), operation time, hospital stay, costs, and complications. Radiologic outcomes included anterior vertebral body height ratio (AVBHR) and Cobb’s angle.
Key Results
• Pain Relief: Intraoperative VAS scores at multiple time points (after anesthesia, during needle puncture, balloon dilation, cement injection, and procedure end) were significantly lower in the TPVB group compared to the LI group (e.g., median VAS at balloon dilation 3 vs. 4; p < 0.05). Postoperative day 1 VAS scores also favored TPVB (median 2 vs. 3; p < 0.05).
• Functional and Quality of Life Outcomes: TPVB patients showed better ODI and SF-36 bodily pain scores at day 1 postoperatively, indicating superior early pain relief and functional recovery. However, these differences were not sustained at longer-term follow-up (3 and 6 months), where both groups showed comparable results.
• Intraoperative Safety: No significant differences were noted in mean arterial pressure or heart rate between groups, with no serious adverse events such as pneumothorax, hemothorax, or epidural spread. The safety profile of TPVB was equivalent to LI.
• Other Parameters: Anesthesia duration was longer in TPVB (23.4 ± 3.95 min) versus LI (6.0 ± 2.77 min), but no differences emerged in surgery duration, hospital stay, costs (p = 0.053, not statistically significant), or cement leakage rates. Radiological outcomes (AVBHR and Cobb's angle) improved similarly in both groups.
Safety Considerations
• TPVB was well tolerated without major complications. Continuous ultrasound guidance minimized risks associated with nerve block placement.
• The hemodynamic stability seen during PKP under TPVB supported its safety.
Limitations
• Single-center with a modest sample size (60 patients) limits generalizability.
• Short-term follow-up restricts assessment of long-term analgesic benefits.
• Results apply to thoracic fractures at T8-T12; efficacy outside this segment remains unclear.
• Indications for TPVB in PKP are not universally established, necessitating further research.
In summary, TPVB provides superior intraoperative and early postoperative analgesia compared to local infiltration with a comparable safety profile in PKP patients with thoracic OVCFs complicated by intercostal neuralgia. Longer-term functional and radiological outcomes were similar. These findings advocate for the use of TPVB as a preferable anesthesia technique in this specific patient population, albeit requiring validation in larger, multicenter trials.
Key Points
• Enhanced Analgesia with TPVB: Thoracic paravertebral nerve block (TPVB) significantly reduced intraoperative pain at all assessed procedural stages (needle puncture, balloon dilation, cement injection) and improved postoperative day 1 pain scores compared to local infiltration (LI) anesthesia in patients undergoing percutaneous kyphoplasty (PKP) for thoracic osteoporotic vertebral compression fractures (OVCFs) with intercostal neuralgia.
• Improved Early Functional Outcomes: Patients receiving TPVB demonstrated superior early postoperative functional recovery, as evidenced by better Oswestry Disability Index (ODI) and SF-36 bodily pain subscale scores on postoperative day 1; however, these differences diminished at 3 and 6 months, with equivalent longer-term functional outcomes between groups.
• Comparable Safety Profiles: No significant differences were observed in intraoperative mean arterial pressure or heart rate between TPVB and LI groups. TPVB was safe with no major complications such as pneumothorax, hemothorax, or epidural spread, aided by continuous ultrasound guidance during nerve block placement.
• Procedure and Resource Use: TPVB required a longer anesthesia administration time (approximately 23 minutes vs. 6 minutes for LI), but this did not affect total surgery duration, hospital length of stay, total costs (which were statistically similar), or rates of cement leakage during PKP.
• Equivalent Radiological Outcomes: Both TPVB and LI groups achieved similar improvements in anterior vertebral body height ratio (AVBHR) and Cobb's angle postoperatively, indicating comparable efficacy in surgical stabilization and deformity correction.
• Study Limitations and Scope: Findings are based on a single-center study with a relatively small sample size of 60 patients and short-term follow-up, limiting generalizability and assessment of long-term analgesic effects. The efficacy and safety conclusions are specific to single-level thoracic (T8-T12) OVCFs, highlighting the need for larger, multicenter trials and research into broader anatomical applicability.
• Reference -
Li Y, Xia H, Chen S, Qian Y, Shen G, Zhong X, Jia Z, Tang C, He S. Thoracic paravertebral block versus local infiltration anesthesia for percutaneous kyphoplasty to treat osteoporotic vertebral compression fractures combined with intercostal neuralgia: a randomized controlled trial. BMC Anesthesiol. 2025 May 19;25(1):253. doi: 10.1186/s12871-025-03114-x. PMID: 40389859; PMCID: PMC12087189.
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


