- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Study Compares IV Propofol and Dexmedetomidine for Awake C-MAC D-Blade-Guided Nasotracheal Intubation
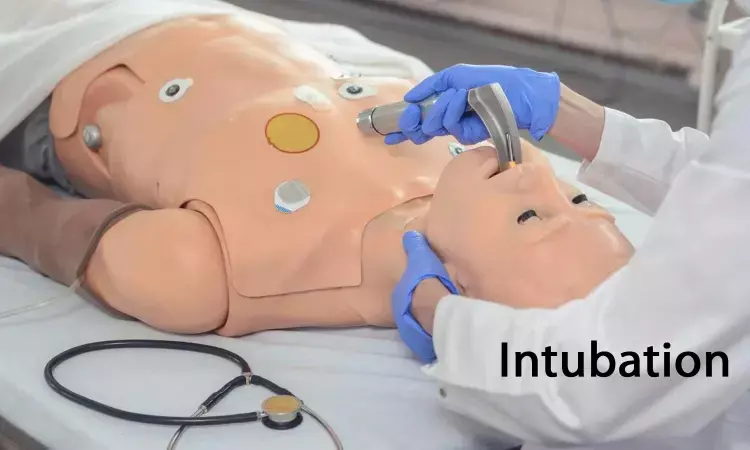
Recent study compared the effectiveness of intravenous (IV) propofol and dexmedetomidine for C-MAC D-blade-guided anticipated difficult nasotracheal intubation under conscious sedation. The study included 60 patients with difficult airways, and after airway preparation with midazolam and fentanyl, patients were randomly assigned to receive propofol or dexmedetomidine for sedation. The primary outcome measure was the intubation score, while secondary outcome measures included haemodynamic parameters, intubation time, number of attempts, glottic view, time to achieve the desired bispectral index (BIS), complications, study drug consumption, and patient-reported satisfaction with the awake intubation technique.
Comparative Results -
The results showed that the intubation score was significantly higher in the dexmedetomidine group compared to the propofol group, indicating better intubation conditions with propofol. Patient reaction to intubation, haemodynamic parameters, and percentage of glottis opening score were more favorable in the propofol group. The time to achieve the desired BIS was four times longer, and the time to intubate was 6 seconds longer in the dexmedetomidine group.
Conclusion on Sedation Options -
The study concluded that successful awake C-MAC® D-blade video laryngoscopic intubation can be performed under dexmedetomidine or propofol conscious sedation, with propofol providing a better intubation score. The authors recommended propofol as the preferred sedation option for successful awake C-MAC® D-blade video laryngoscopic intubation.
Study Limitations and Recommendations -
The study had some limitations, such as using a specific video laryngoscope and the skill-dependent nature of the results, but it provided valuable insights into the comparison of propofol and dexmedetomidine sedation for awake video laryngoscopic intubation in patients with difficult airways. The authors suggested conducting multicentric, randomised controlled trials using different video laryngoscopes to further compare the efficacy of various sedatives for awake nasotracheal intubation in anticipated difficult airways.
In conclusion, the study demonstrated that propofol and dexmedetomidine can both provide good intubation conditions for awake C-MAC® D-blade video laryngoscopic intubation, but propofol was found to offer better intubation scores, patient reaction, and haemodynamic parameters.
Key Points
- The study compared the effectiveness of intravenous (IV) propofol and dexmedetomidine for awake C-MAC® D-blade-guided anticipated difficult nasotracheal intubation under conscious sedation in 60 patients with difficult airways. After airway preparation, patients were randomly assigned to receive either propofol or dexmedetomidine for sedation. The primary outcome measure was the intubation score, and secondary outcome measures included haemodynamic parameters, intubation time, number of attempts, glottic view, time to achieve the desired bispectral index (BIS), complications, study drug consumption, and patient-reported satisfaction with the awake intubation technique.
- The results indicated that the intubation score was significantly higher in the propofol group compared to the dexmedetomidine group, suggesting better intubation conditions with propofol. Additionally, patient reaction to intubation, haemodynamic parameters, and percentage of glottis opening score were more favorable in the propofol group. The time to achieve the desired BIS was four times longer, and the time to intubate was 6 seconds longer in the dexmedetomidine group.
- The study concluded that both dexmedetomidine and propofol can be used for successful awake C-MAC® D-blade video laryngoscopic intubation, but propofol provided a better intubation score. The authors recommended propofol as the preferred sedation option for awake C-MAC® D-blade video laryngoscopic intubation. The study recognized limitations, such as using a specific video laryngoscope and the skill-dependent nature of the results, and recommended further multicentric, randomised controlled trials using different video laryngoscopes to compare the efficacy of various sedatives for awake nasotracheal intubation in patients with difficult airways.
Reference –
Vishnoi G, Shah SB, Chawla R, Bhardwaj M, Patel A, Arora J. Comparison of propofol versus dexmedetomidine sedation for awake C‑MAC® D‑Blade video laryngoscopic nasotracheal intubation in patients with difficult airway: A randomised clinical study. Indian J Anaesth 2024;68:699‑705
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.


