- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
CABG 2-3 days after ticagrelor cessation is safe: RAPID CABG trial
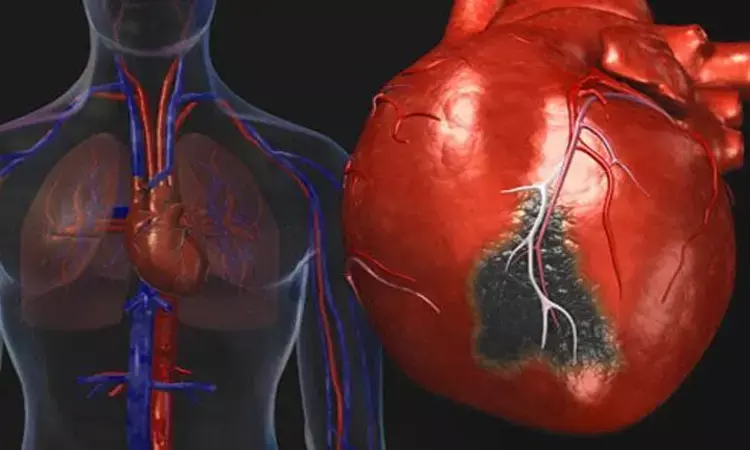
USA: A small, randomized study of people who had heart attacks demonstrated no increased risk of bleeding when ticagrelor was stopped 2-3 days before coronary artery bypass surgery (CABG). This may enable patients to go to bypass surgery sooner and this, in turn, may decrease hospital length of stay.
According to results from the RAPID CABG trial, early bypass surgery performed 2 to 3 days after ticagrelor cessation is noninferior to delayed CABG performed at 5 to 7 days in regards to the outcome of severe or massive perioperative bleeding in ACS patients who required nonemergent surgery. The results from the late-breaking research were presented at the American Heart Association's Scientific Sessions 2021.
"We discovered no significant increase in bleeding when people had bypass surgery after 2-3 days of discontinuing ticagrelor," said lead study author Derek So, M.D, a cardiologist at the University of Ottawa Heart Institute and a professor at the University of Ottawa in Canada. "These findings may be surprising based on the assumption that the presence of a strong blood thinner should predispose people to severe bleeding."
Ticagrelor is a common antiplatelet medication prescribed for preventing blood clots after a heart attack. However, it should be stopped prior to surgery due to the risk of bleeding as ticagrelor is a blood thinner. About 10% of patients with heart attacks require CABG. Current American Heart Association (AHA) guidelines recommend people who take ticagrelor and need bypass surgery should stop taking the medicine 5-7 days before surgery.
To evaluate if a shorter waiting time for surgery after stopping ticagrelor is safe, the "Reassessment of Anti-Platelet Therapy Using InDividualized Strategies - Ticagrelor in Patients With Acute Coronary Syndromes Treated by Coronary Artery Bypass Graft Surgery (RAPID CABG)" trial assessed bleeding after bypass surgery in people at two centers in Canada. The study investigators randomly assigned 143 people who previously had suffered heart attacks, had received ticagrelor and required bypass surgery into two groups – one for earlier surgery after stopping ticagrelor and the other for surgery after the standard wait time.
A total of 72 people (average age of 64 years, 80.6% male) were in the early bypass surgery group and had surgery 2-3 days after stopping ticagrelor, and 71 people (average age of 65.5 years, 83.1% male) were in the delayed surgery group, following current standard of care of stopping ticagrelor 5-7 days before surgery. The people in both groups had similar baseline characteristics, including age and percentages of coexisting health conditions.
Study researchers gauged the number of people who had severe or massive perioperative bleeding during the early post-surgical period, as defined by the universal definition of perioperative bleeding (UDPB). Severe or massive bleeding defined by UDPB includes massive blood transfusions of >5 units of red cells or plasma within 24 hours of surgical closure, chest tube drainage of over 1000 mL in the first 12 hours and re-operation for bleeding. The investigators also compared the length of stay in the hospital and rates of episodes of angina, recurrent heart attack, stroke and death among the two groups.
Key findings include:
- Bypass surgery in the early surgery group (after 2-3 days of stopping ticagrelor) showed no increased risk of early post-surgical bleeding, and rates of bleeding were similar between the two groups.
- The rate of severe or massive perioperative bleeding (using the universal definition of perioperative bleeding) was 4.6% in the early surgery group and 5.2% in the delayed group. For clinical reasons, some people in the delayed surgery group had to have CABG surgery sooner than the planned date; 9% experienced recurrent angina (chest pains), recurrent heart attack and ventricular arrhythmias (abnormal rhythms which may be due to the blockages) that prompted earlier surgery.
- In contrast, no one in the early surgery group had to have surgery earlier than two days after they stopped taking ticagrelor.
- The average length of hospital stay was reduced by 3 days among the participants in the early surgery group compared to the delayed surgery group.
"Research such as this, with people randomly allocated to early vs. delayed surgery, is integral to assure cardiologists and surgeons that early surgery is safe, especially since it conflicts with the present guidelines for people who are taking ticagrelor," So said. "Furthermore, although our study was not large enough to evaluate whether early surgery protects people from suffering early recurrent heart attacks or angina, it opens this hypothesis and may prompt future research in the area."
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


