- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
GLS improves risk stratification in heart failure patients, MyoVasc study
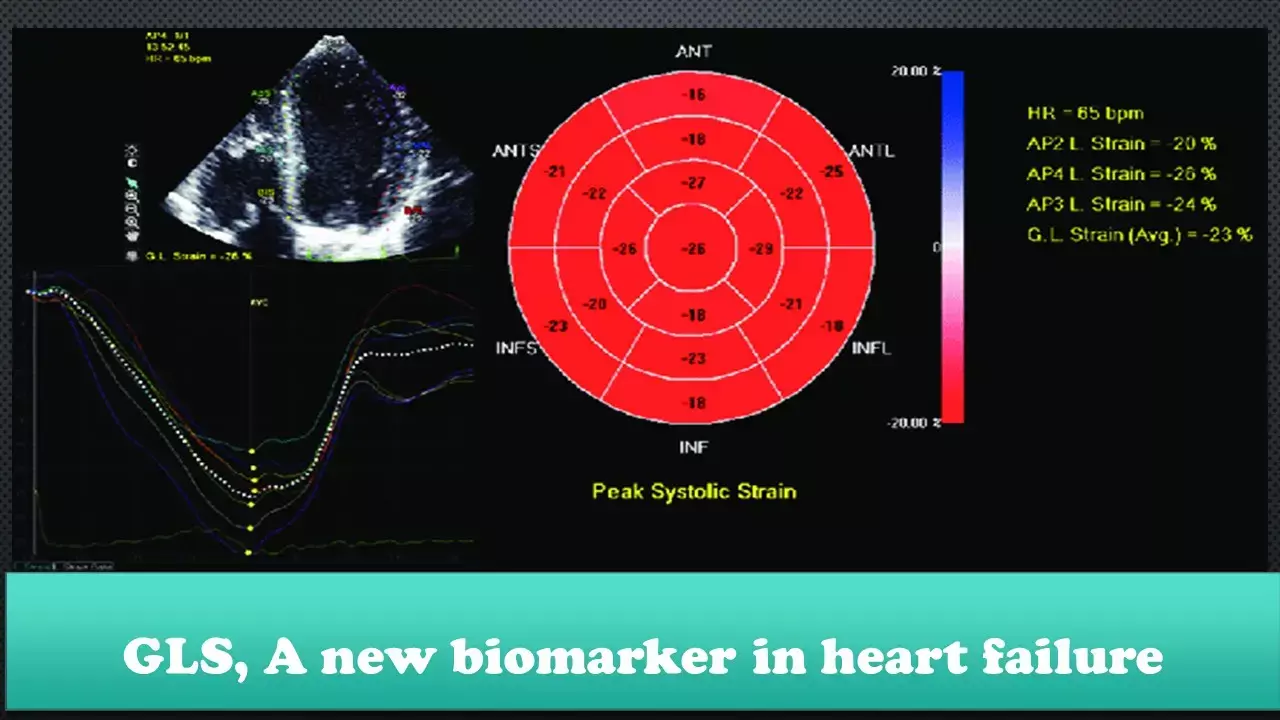
Left ventricular ejection fraction (LVEF) is the most conventional clinical parameter for heart failure (HF) patients but has its own limitations. Global longitudinal strain (GLS) addresses most of these shortcomings and is rapidly emerging as a new biomarker for HF patients.
In a recent study published in JAMA cardiology, Trobe et al have shown that in patients with chronic HF, GLS was associated with clinical and cardiac status, reflected neurohormonal activation, and was associated with cardiac mortality independent of clinical and cardiac status. This is the largest prospective study of patients with chronic HF to evaluate GLS in the full range of the HF syndrome, from asymptomatic to symptomatic HF.
The factors associated with GLS in the setting of chronic HF have not been studied extensively. To date, evidence is limited to investigations in small studies and no comprehensive evaluation of factors associated with GLS is available for patients with HF. Against this background, the present study aimed to (1) investigate the clinical factors associated with GLS in the HF syndrome, (2) provide insights into the interdependence of GLS with established markers of cardiac systolic and diastolic function and N-terminal prohormone B-type natriuretic protein (NTproBNP) as the standard laboratory biomarker of HF, and (3) broadly assess the association of GLS with cardiac and all-cause mortality.
The observational, prospective study enrolled 3289 individuals with asymptomatic to symptomatic HF. The median follow-up was 3.2 years (interquartile range, 2.0-4.0 years). Participants with stages A to D HF according to American Heart Association (AHA) criteria were examined at a dedicated study center. Echocardiography was performed with GLS measurement by independent reviewers.
In the study sample, data on GLS were available on 2440 individuals, of whom 2186 were classified as having AHA HF stages A to D. Mean (SD) GLS worsened across AHA stages from stage A (n = 434; −19.44 [3.15%]) to stage B (n = 629; −18.01 [3.46%]) to stages C/D (n = 1123; −15.52 [4.64%]), female sex, obesity, atrial fibrillation, myocardial infarction and estimated glomerular filtration rate were independently associated with GLS in multivariable regression analysis.
GLS was associated with the severity of HF as reflected by N-terminal prohormone B-type natriuretic protein (NT-proBNP) levels after additionally adjusting for cardiac structure and function. During follow-up, GLS was associated with all-cause and cardiac death independent of image quality, observer variability, clinical profile, HF medications, NYHA class, and cardiac structure and function. After further adjustment for the NT-proBNP level, GLS remained associated with cardiac death but not all-cause mortality.
The main findings of this study suggest that
(1) male sex, obesity, hemoglobinA1c, atrial fibrillation, coronary artery disease, and a history of myocardial infarction are the major independent clinical factors associated with higher GLS in individuals with HF;
(2) GLS is associated with the severity of HF as reflected by NT-proBNP levels independent of the clinical profile, NYHA class, and measures of cardiac structure and function;
(3) GLS is associated with echocardiographic measures of structure and function, but independent of the clinical profile only for LVMi, diastolic function as reflected by E/E′ ratio, and systolic function as reflected by LVEF, with the strongest association detected with LVEF; and
(4) GLS is associated with cardiac death and all-cause mortality in patients with HF independent of the clinical profile and cardiac structure and function.
Thus, GLS may serve as a useful tool to improve risk stratification in patients with HF.
Source: JAMA cardiology. doi:10.1001/jamacardio.2020.7184
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


