- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
OCT guidance not superior to conventional angio-guided PCI in improving clinical outcomes, ILUMIEN-IV trial.
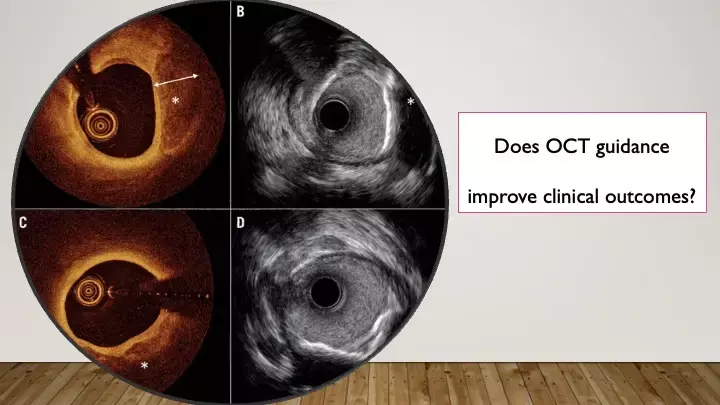
Data regarding clinical outcomes after optical coherence tomography (OCT)-guided percutaneous coronary intervention (PCI) as compared with angiography-guided PCI are limited. To address this gap in literature, authors Ali et al have now published the results of the recently conducted ILUMIEN-IV trial in NEJM this week. This study shows that among patients undergoing PCI, OCT guidance does not prove superior to angiography-guided PCI in improving target-vessel failure at 2 years.
The study hypothesis is based on the conventional 30-year-old theory of interventional cardiology: that the establishment of the largest final coronary luminal diameter results in the lowest risk of repeat coronary revascularization. Hence OCT guidance that serves to achieve better luminal gains is hypothesized to improve clinical outcomes.
In this prospective, randomized, single-blind trial, they randomly assigned patients with medication-treated diabetes or complex coronary-artery lesions to undergo OCT-guided PCI or angiography-guided PCI.
A final blinded OCT procedure was performed in patients in the angiography group. The two primary efficacy end points were the minimum stent area after PCI as assessed with OCT and target-vessel failure at 2 years, defined as a composite of death from cardiac causes, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization.
A total of 2487 patients wre enrolled: 1233 patients were assigned to undergo OCT-guided PCI, and 1254 to undergo angiography-guided PCI. The minimum stent area after PCI (5.72±2.04 mm2) in the OCT group was significantly more than that achieved with angiography alone (5.36±1.87 mm2).a
But, target-vessel failure within 2 years occurred with a non-significant difference between the two groups.
Stent thrombosis within 2 years occurred in 0.5% in the OCT group and in 1.4% in the angiography group.
In addition, OCT guidance resulted in a lower frequency of severe dissection, major stent malapposition, major tissue protrusion, and untreated focal reference segment disease.
Does the negative result in the ILUMIEN IV trial indicate that a foundation of interventional cardiology — that larger acute coronary lumen gains improve patient outcomes — may no longer broadly apply in the era of contemporary drug-eluting stents and pharmacology? Is this theory only valid when the more macroscopic assessment of luminal changes assessed by angiography is used? These are some of the questions that need to be explored in further trials.
Other recent trials comparing the impact of imaging on clinical outcomes have yielded positive results. These include the simultaneously published OCTOBER trial and RENOVATE COMPLEX-PCI trials. One might simply conclude that the directionally favorable safety end point of the ILUMIEN IV trial (stent thrombosis) in conjunction with the positive primary clinical end points of the OCTOBER and RENOVATE-COMPLEX-PCI trials strengthen the mandate for a class effect of intracoronary imaging as a necessary method to improve PCI outcomes across a broad spectrum of patients and coronary-artery lesions.
Source: NEJM: DOI: 10.1056/NEJMoa230586
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


