- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Online 3D-OFDI-guided PCI bests angiography-guided PCI in bifurcation lesions
Percutaneous coronary intervention (PCI) with drug-eluting stent (DES) implantation is a common revascularization method for coronary artery disease with appropriate complexity of the disease.
Recent trial findings published in the Circulation: Cardiovascular Interventions suggests the rate of acute incomplete stent apposition at bifurcation was lower with online 3-dimensional optical frequency domain imaging (3D-OFDI) guided bifurcation PCI than with angiography-guided bifurcation PCI.
Coronary bifurcation lesions account for 15% to 20% of all patients undergoing PCI. The current guidelines for myocardial revascularization of coronary bifurcations recommend a provisional one stent strategy as a default stenting technique. Previous retrospective data and published case reports on novel imaging technique (online 3D-OFDI) have suggested that it is feasible to perform online visualization of the bifurcation rewiring position and that this approach can improve acute outcomes such as incomplete stent apposition (ISA). However, additional OFDI pullback step in the catheterization laboratories will increase the amount of total contrast volume as well as procedural time for the patients. The efficacy of online 3D-OFDI-guided PCI in the reduction of ISA has not yet been investigated prospectively in the context of a randomized controlled trial. For this purpose, researchers conducted OPTIMUM trial to determine whether online 3D-OFDI-guided stenting is superior to angiography-guided percutaneous coronary intervention (PCI) in terms of incomplete stent apposition at the bifurcation segment.
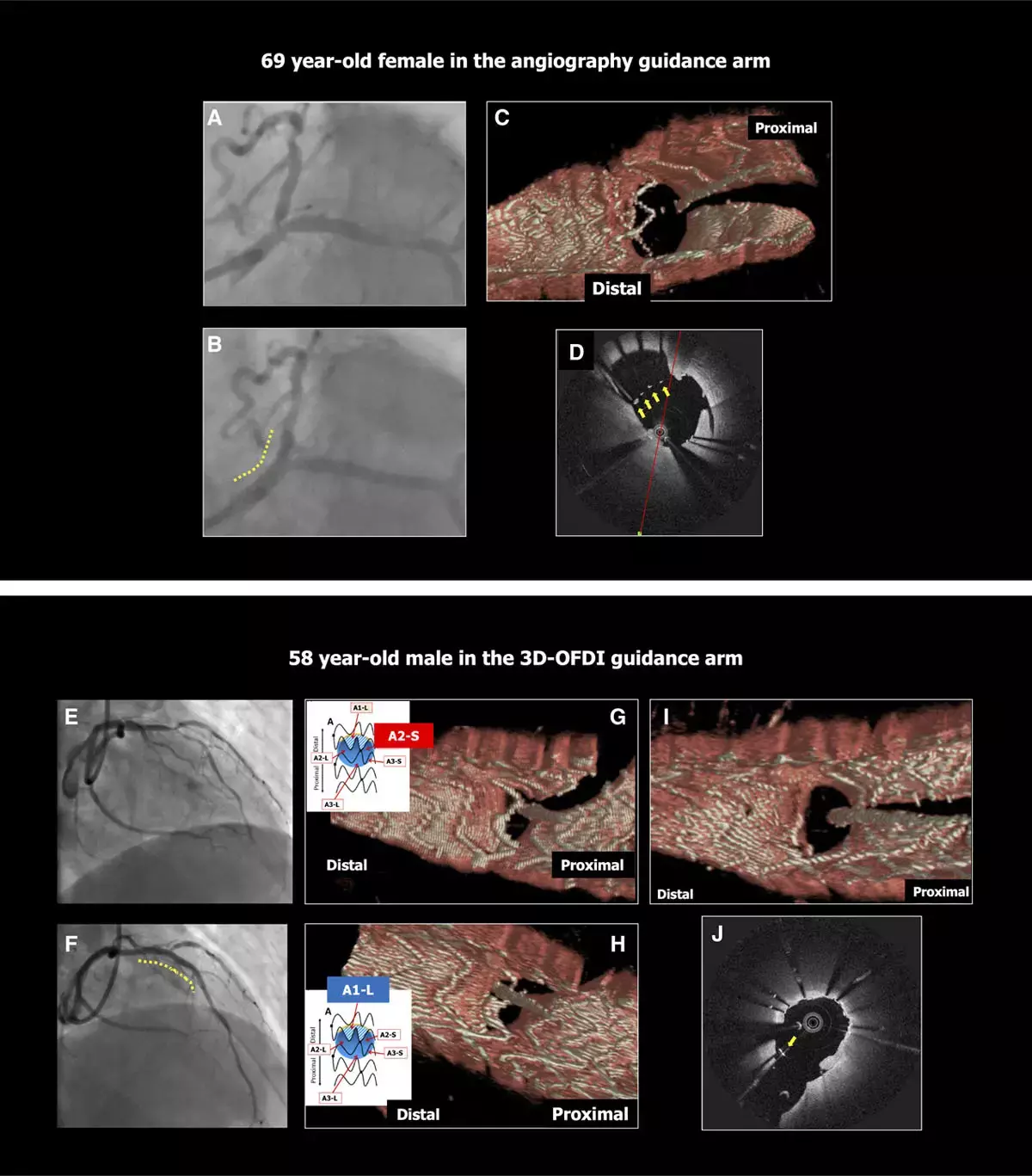
The OPTIMUM trial (Online 3-Dimensional Optical Frequency Domain Imaging to Optimize Bifurcation Stenting Using UltiMaster Stent) was the first prospective, randomized, active control, superiority, multicenter clinical trial across 4 Japanese canters to evaluate the efficacy and safety of the on-line 3D-OFDI guided PCI. A total of 110 patients with 111 bifurcation lesions were randomized among which 56 patients with 57 lesions were treated with 3D-OFDI-guided PCI, whereas 54 patients with 54 lesions were treated with angiography-guided PCI between June 8, 2017, and September 26, 2018. They had angiographically significant stenosis in the bifurcation lesion treated with a provisional single stent strategy using the Ultimaster sirolimus-eluting stent. Patients randomized to 3D-OFDI guidance underwent online 3D-OFDI assessment after rewiring into the jailed side branch after stenting and proximal optimization technique, while in the angiography guidance arm, rewiring was performed using conventional fluoroscopic/angiographic guidance. The major outcome assessed was the postprocedural average percentage of mal-apposed struts per lesion assessed by OFDI in the confluence zone of the main and side branches.
Upon analysis researchers have found in the 3D-OFDI guidance arm, the feasibility of online 3D-OFDI was 98.2%. They also found the average percentage of incomplete stent apposition per lesion at bifurcation was lower in the 3D-OFDI guidance arm than that in the angiography guidance arm (19.5±15.8% versus 27.5±14.2%). They also confirmed the superiority of the 3D-OFDI guidance arm in the strut level analysis (odds ratio: 0.54).
The authors concluded, "In a series of predominantly non-LM bifurcation lesions, online 3D-OFDI-guided PCI demonstrated excellent feasibility and was superior to angiography guidance in reducing acute ISA at the bifurcation. Three-dimensional-OFDI imaging guidance may therefore be preferable in bifurcation PCI. Further trials are warranted to confirm the long-term clinical benefit of these favourable mechanical findings".
For further information:
https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.120.009183
Medical Dialogues Bureau consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


