- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
PCI in setting of severe LV dysfunction does not improve survival or HF hospitalizations: NEJM study
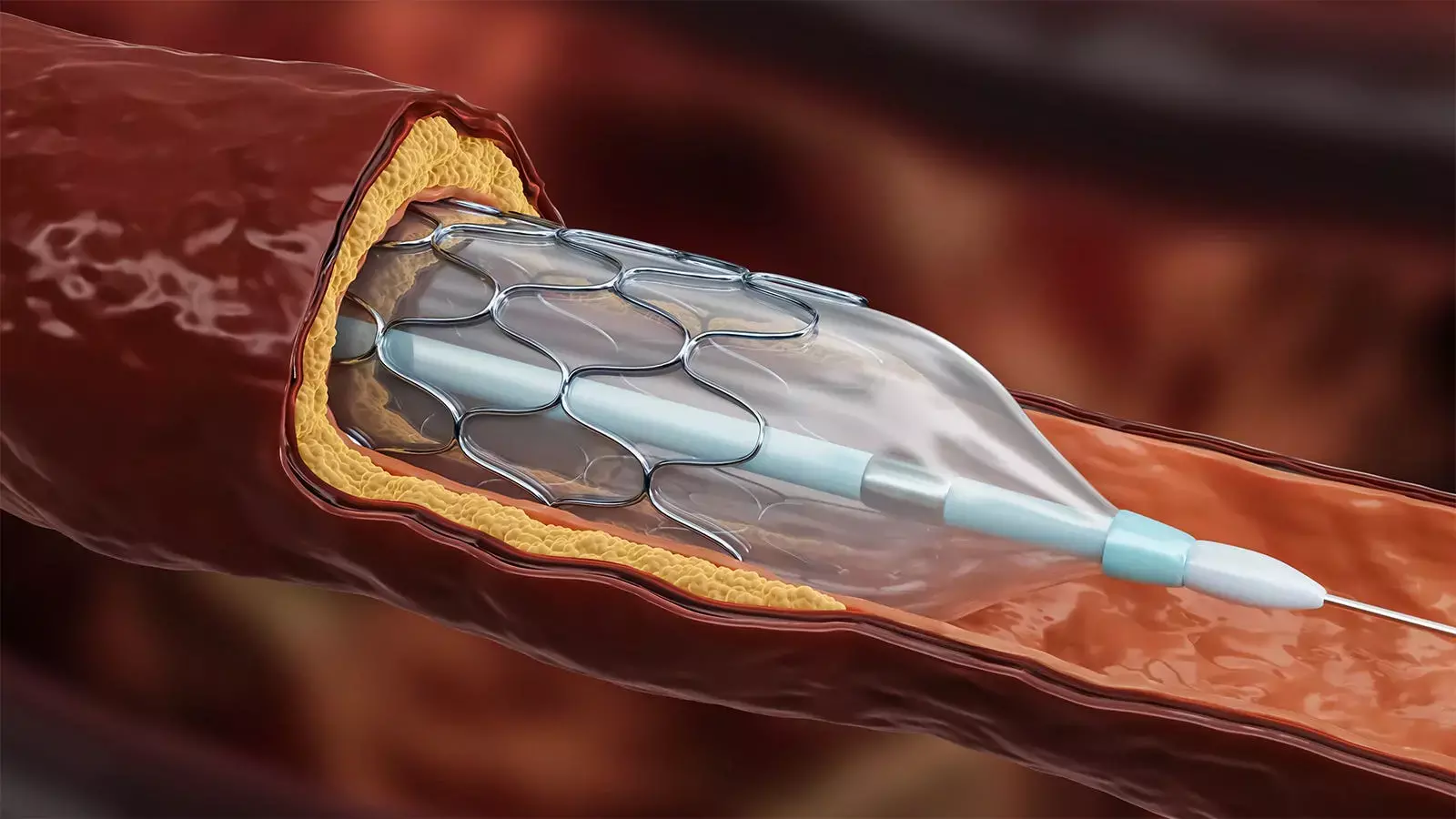
Whether revascularization by PCI can improve event-free survival and LV function in patients with severe ischemic LV systolic dysfunction, as compared with optimal medical therapy alone, is unknown. Contrary to the results of STICH trial that showed benefit of surgical revascularisation in this setting, the results of REVIVED-BCIS2 trial published recently in NEJM have shown no benefit of PCI in reducing all-cause mortality and HF hospitalization. However, the Quality-of-life scores at 6 and 12 months appeared to favor the PCI group.
PCI is an alternative mode of revascularization, but most randomized comparisons between CABG and PCI among patients with chronic coronary syndromes have excluded patients with severe left ventricular systolic dysfunction. Whether PCI might allow the benefits of revascularization to be realized without the early hazard associated with CABG in patients with ischemic left ventricular dysfunction is not known.
To explore the possibility of a comparable benefit with PCI in this subset of patients, REVIVED-BCIS2 investigators randomly assigned patients with a left ventricular ejection fraction of 35% or less, extensive coronary artery disease amenable to PCI, and demonstrable myocardial viability to a strategy of either PCI plus optimal medical therapy (PCI group) or optimal medical therapy alone (optimal-medical-therapy group).
The primary composite outcome was death from any cause or hospitalization for heart failure. Major secondary outcomes were left ventricular ejection fraction at 6 and 12 months and quality-of-life scores.
Over a median of 41 months, a primary-outcome event occurred in 37.2% in the PCI group and 38.0% in the optimal-medical-therapy group.The left ventricular ejection fraction was similar in the two groups at 6 months and at 12 months. Quality-of-life scores at 6 and 12 months appeared to favor the PCI group, but the difference had diminished at 24 months.
However, there were no signs of diverging or improved outcomes with PCI over a median follow-up of 3.4 years, a finding that differed from what was observed with surgical revascularization in the STICH trial and that was later confirmed in its extension trial.
"More than anything, this trial supports the importance of guideline-directed medical therapies for the management of left ventricular dysfunction, irrespective of whether revascularization is considered. The observed increases in the ejection fraction and the relatively low percentage of patients with hospitalization for heart failure in both treatment groups would only be expected to improve further with the use of more contemporary therapies for congestive heart failure" notes Ajay J. Kirtane, M.D in an accompanying editorial.
While the results of requisite additional analyses and follow-up data from the REVIVED trial are awaited, the prevailing dictum should be to diagnose the joint conditions of CHF and CAD and to provide therapies that are known to be effective for both of these conditions.
Source: NEJM:
1. DOI: 10.1056/NEJMoa2206606
2. DOI: 10.1056/NEJMe2210183
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


