- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Revacept doesn't reduce myocardial injury risk in patients undergoing PCI: JAMA
Germany: The addition of revacept to standard antithrombotic therapy in patients with stable ischemic heart disease (SIHD) undergoing PCI, does not reduce the risk of myocardial injury (MI), show results from the ISAR-PLASTER Phase 2 Trial. The study findings are published in the journal JAMA Cardiology.
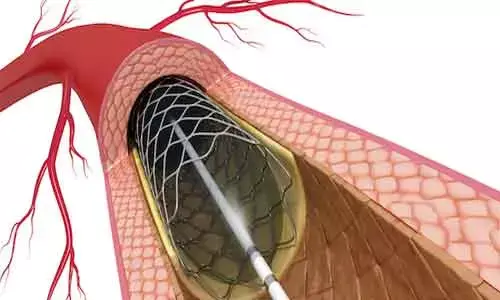
Patients undergoing percutaneous coronary intervention (PCI) for acute coronary syndromes (ACS) or SIHD receive dual antiplatelet therapy (DAPT). DAPT consists of a combination of aspirin and a P2Y12 inhibitor for preventing periprocedural and postprocedural ischemic events. Despite DAPT use, patients continue to experience periprocedural ischemic events, which represent independent and strong predictors for unfavorable outcomes including mortality.
Considering the above background, Katharina Mayer, Technical University of Munich, Munich, Germany, and colleagues aimed to test the safety and efficacy of revacept, a novel, lesion-directed antithrombotic drug, acting as a competitive antagonist to platelet glycoprotein VI in randomized, double-blind, placebo-controlled ISAR-PLASTER phase 2 trial.
The study enrolled patients from 9 centers in Germany from November 20, 2017, to February 27, 2020; follow-up ended on March 27, 2020. 334 patients with SIHD undergoing PCI were included. They were randomized to receive either a single intravenous infusion of revacept, 160 mg, revacept (n-120), 80 mg (n=121), or a placebo (n=93) prior to the start of PCI on top of standard antithrombotic therapy.
The primary endpoint was the composite of death or myocardial injury, defined as an increase in high-sensitivity cardiac troponin to at least 5 times the upper limit of normal within 48 hours from randomization.
The study yielded the following key findings:
- The primary end point showed no significant differences between the revacept and placebo groups: 24.4%, 25.0%, and 23.3% in the revacept, 160 mg, revacept, 80 mg, and placebo groups, respectively.
- The high dose of revacept was associated with a small but significant reduction of high-concentration collagen-induced platelet aggregation, with a median 26.5 AU × min (interquartile range, 0.5-62.2 AU × min) in the revacept, 160 mg, group; 43.5 AU × min (interquartile range, 22.8-99.5 AU × min) in the revacept, 80 mg, group; and 41.0 AU × min (interquartile range, 31.2-101.0 AU × min) in the placebo group, while adenosine 5′-diphosphate–induced aggregation was not affected.
- Revacept did not increase Bleeding Academic Research Consortium type 2 or higher bleeding at 30 days compared with placebo: 5.0%, 5.9%, and 8.6% in the revacept, 160 mg, revacept, 80 mg, and placebo groups, respectively.
"Our findings revealed that revacept did not reduce myocardial injury in patients with stable ischemic heart disease undergoing percutaneous coronary intervention," wrote the authors. "There were few bleeding events and no significant differences between treatment arms."
Reference:
The study titled, "Efficacy and Safety of Revacept, a Novel Lesion-Directed Competitive Antagonist to Platelet Glycoprotein VI, in Patients Undergoing Elective Percutaneous Coronary Intervention for Stable Ischemic Heart Disease: The Randomized, Double-blind, Placebo-Controlled ISAR-PLASTER Phase 2 Trial," is published in the journal JAMA Cardiology.
DOI: https://jamanetwork.com/journals/jamacardiology/fullarticle/2777812
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


