- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Awake Prone Positioning on Endotracheal Intubation in Patients With COVID-19 not so effective: JAMA
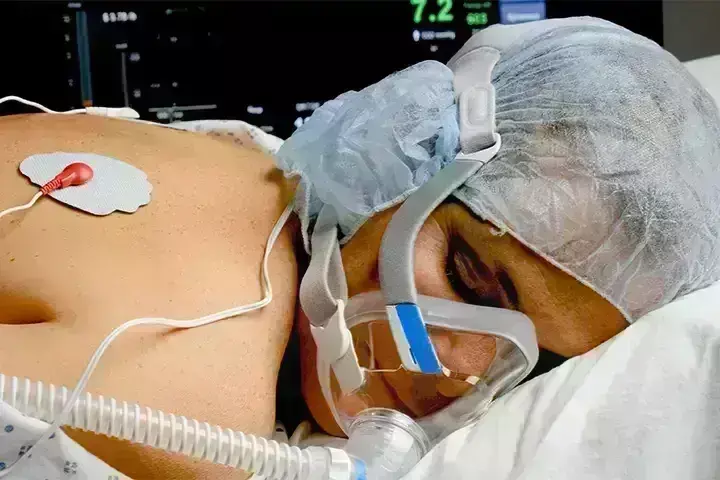
In patients with acute hypoxemic respiratory failure from COVID-19, prone positioning, compared with usual care without prone positioning, did not significantly reduce endotracheal intubation at 30 days, a recent trial published in JAMA has found.
Hospitalizations due to COVID-19 strained critical care resources internationally.
Prone positioning has been used since the 1970s in patients undergoing invasive mechanical ventilation for acute respiratory distress syndrome.
Observational studies showed that prone positioning may result in increased lung volume, homogenized pleural pressure, and reduced shunting.
Furthermore, randomized clinical trials found prone positioning to be associated with a lower risk of death in patients undergoing invasive mechanical ventilation for moderate to severe acute respiratory distress syndrome.
The COVI-PRONE (Awake Prone Position in Hypoxemic Patients with Coronavirus Disease 19) trial, conducted by Waleed Alhazzani et. al aimed to assess the efficacy and adverse events of awake prone positioning in patients who were not intubated and who had COVID-19 with hypoxemic respiratory failure.
A pragmatic, unblinded randomized clinical trial was conducted at 21 hospitals in Canada, Kuwait, Saudi Arabia, and the US.
Eligible adult patients with COVID-19 were not intubated and required oxygen (≥40%) or noninvasive ventilation. A total of 400 patients were enrolled between May 19, 2020, and May 18, 2021, and the final follow-up was completed in July 2021.
Patients were randomized to awake prone positioning or usual care without prone positioning.
Among the 400 patients who were randomized 117 [29.3%] were women), and all (100%) completed the trial.
In the first 4 days after randomization, the median duration of prone positioning was 4.8 h/d in the awake prone positioning group vs 0 h/d in the control group.
By day 30, 70 of 205 patients (34.1%) in the prone positioning group were intubated vs 79 of 195 patients (40.5%) in the control group.
The researchers found that prone positioning did not significantly reduce mortality at 60 days and had no significant effect on days free from invasive mechanical ventilation or noninvasive ventilation at 30 days or on days free from the intensive care unit or hospital at 60 days.
They also found that:
There were no serious adverse events in either group.
In the awake prone positioning group, 21 patients (10%) experienced adverse events and the most frequently reported were musculoskeletal pain or discomfort from prone positioning (13 of 205 patients [6.34%]) and desaturation (2 of 205 patients [0.98%]).
There were no reported adverse events in the control group.
"In patients with acute hypoxemic respiratory failure from COVID-19, prone positioning, compared with usual care without prone positioning, did not significantly reduce endotracheal intubation at 30 days. However, the effect size for the primary study outcome was imprecise and does not exclude a clinically important benefit," the authors concluded.
For the full article : doi:10.1001/jama.2022.7993
B.Sc Life Sciences, M.Sc Biotechnology, B.Ed
Isra Zaman is a Life Science graduate from Daulat Ram College, Delhi University, and a postgraduate in Biotechnology from Amity University. She has a flair for writing, and her roles at Medicaldialogues include that of a Sr. content writer and a medical correspondent. Her news pieces cover recent discoveries and updates from the health and medicine sector. She can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


