- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Enzymatic cleaners fail to decontaminate and establish sterile surface in used healing abutments: Study
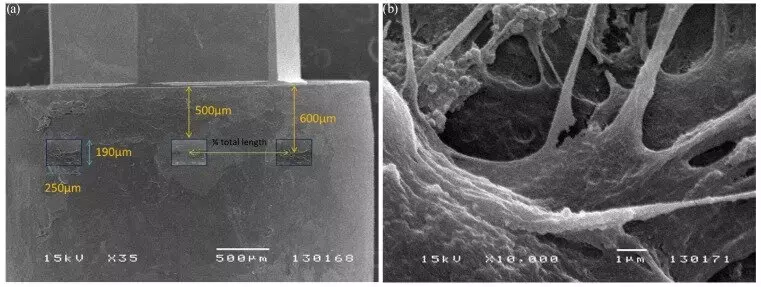
A study was done to evaluate four decontamination strategies utilizing enzymatic agents available in most clinical settings to determine (1) the amount of biomaterial that can be removed in a group of previously used healing abutments (uHAs) and (2) the degree to which the decontaminated healing abutments are capable of inducing an inflammatory response in vitro compared to new healing abutments. In total, 50 healing abutments were collected following 2 to 4 weeks of intraoral use and distributed randomly into five test groups (groups A–E; n = 10 per group). Group A used enzymatic cleaner foam and an autoclave. Group B used an ultrasonic bath with enzymatic cleaner and an autoclave. Group C used a prophy jet, enzymatic cleaner foam, and an autoclave. Group D used a prophy jet, an ultrasonic bath with an enzymatic cleaner, and an autoclave. Lastly, group E used a prophy jet and an autoclave.
The control group consisted of 10 new and sterile HAs. Residual protein concentration was determined by a Micro BCA protein assay (Thermo Fisher Scientific) while healing abutments from each group were stained with Phloxine B and macroscopically examined for the presence of debris. Human primary macrophages were exposed to healing abutments to examine the inflammatory potential, and supernatant levels of nine cytokine and chemokine profiles were analyzed using a multiplex bead assay.
Results: All test groups showed differences in the degree of visual decontamination compared to controls. Groups D and E displayed the most effective surface debris removal and reduced protein concentration, while group A was the least effective. However, compared to controls, all test groups showed high levels of inflammatory cytokine secretion via multiplex assay for up to 5 days. The study found that decontaminating used healing abutments utilizing enzymatic cleaners failed to reestablish inert healing abutment surfaces and prevent an inflammatory immune response in vitro. Clinicians should not reuse healing abutments even after attempts to decontaminate and sterilize healing abutments surfaces.
Reference:
Abreu OJ, Estepa AV, Naqvi AR, Nares S, Narvekar A. Assessment of Detoxification Strategies for Used Dental Implant Healing Abutments: Macroscopic and Biologic Implications. Int J Oral Maxillofac Implants. 2024 Aug 29;39(4):516-525. doi: 10.11607/jomi.10651. PMID: 37910839.
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


