- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Psoriasis Treatments Show No Impact on Blood Glucose Levels: Study
A new study published in Dermatology just put to rest the idea that biologics or methotrexate might double as anti-diabetes medications for people with psoriasis. Researchers tracked HbA1c levels in 386 psoriasis patients over the course of a year—those treated with TNF-α inhibitors (like adalimumab and infliximab), IL-17 inhibitors (brodalumab, ixekizumab, secukinumab), IL-12/23 inhibitor (ustekinumab), IL-23 inhibitors (guselkumab, risankizumab), and methotrexate. Across all treatment groups, HbA1c values stayed essentially unchanged. A tiny increase seen with secukinumab was deemed not clinically significant. Even when the analysis focused only on patients with higher initial HbA1c (36–47 mmol/mol), treatment had zero impact.
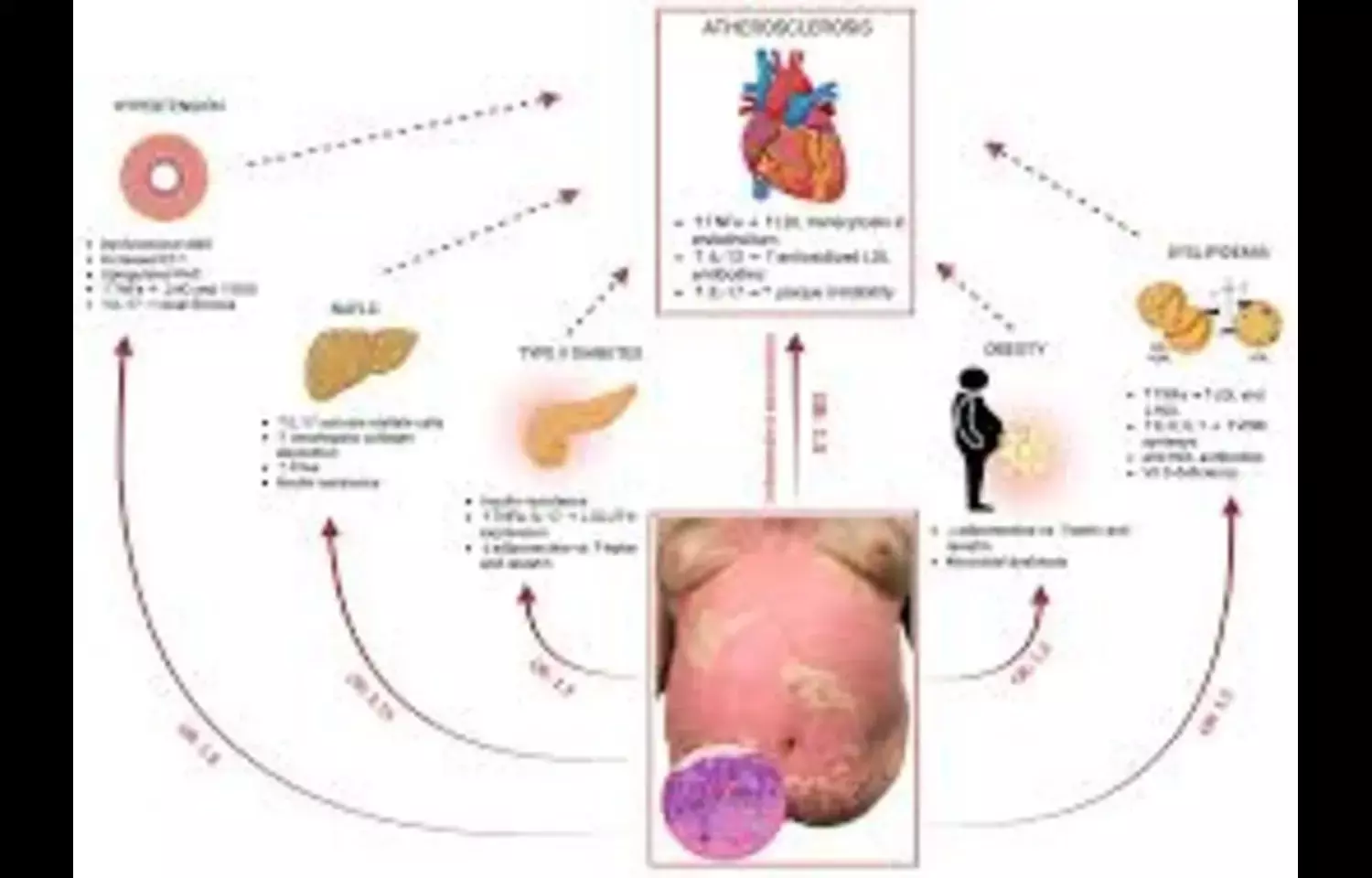
Why does this matter? People with psoriasis generally run a higher risk of developing type-2 diabetes—likely tied to chronic inflammation. It’s tempting to hope that anti-inflammatory biologics or methotrexate could pull double duty by improving glucose metabolism. But this study’s data suggest otherwise: these effective skin-clearing treatments don’t seem to nudge blood sugar.
That doesn’t mean biologics aren’t valuable—they still work wonders for managing skin symptoms and overall inflammation. But for diabetics, or psoriasis patients concerned about long-term metabolic risks, it’s important to know these drugs don’t appear to offer glycemic protection.
For clinicians, this means continuing to monitor HbA1c routinely, just like in any other patient, and pushing for proven metabolic strategies—diet, exercise, medications when needed—rather than assuming psoriasis treatment alone will move the needle.
Keywords: psoriasis, biologic therapy, methotrexate, HbA1c, glucose metabolism, antidiabetic effect, Dermatology journal
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.


