- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Cervical lymphadenopathy- Standard Treatment Guidelines By Government Of India
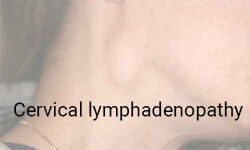
Lymphadenopathy is an abnormal increase in size and/ or altered consistency of lymph nodes. It is a clinical manifestation of regional or systemic disease and serves as an excellent clue to the underlying disease. Cervical lymphadenopathy (C.L.) is a fairly common clinical presentation.
Ministry of Health and Family Welfare Government of India has released the standard treatment guidelines on Cervical Lymphadenopathy. Following are its major recommendations
Surgical anatomy and classification - Cervical lymph nodes are lymph nodes found in the neck. There are approximately 300 lymph nodes in the neck Cervical lymph nodes are classifieds into 7 groups. They are-
· Level I: Submental and submandibular nodes
· Level Ia: Submental triangle
· Level Ib: Submandibular triangle
· Level II: Upper jugular nodes
· Level III: Middle jugular nodes
· Level IV: Lower jugular nodes
· Level V: Posterior triangle group
· Level VI: Pre-tracheal, pre-laryngeal and post-tracheal
· Level VII: Mediastinal
Incidence-
- Age < 30 - 79% benign; 15% lymphomatous; 6% carcinomas
- Age > 50 - 40% benign; 16% lymphomatous; 44% carcinomas
- 0.6 annual incidence of generalized lymphadenopathy
Differential diagnosis-
Common infectious causes of lymphadenopathy
1. Adenovirus
2. CMV
3. Enterovirus
4. EBV
5. Varicella
6. Herpes simplex
7. Staphlococcus infection
8. Group A hemolytic Streptococcus
9. Tularemia
10. Brucellocis
11. Tuberculosis
12. Atypical mycobacteria
13. Klebsilla
14. AIDS
15. Bubonic plague
16. Anthrax
Common non-infectious causes of lymphadenopathy
1. Hodgkin's disease
2. Lymphomas
3. Leukemia
4. Metastatic disease
5. Histiocytosis
6. SLE and JRA
7. Kawasaki Disease
8. Sarcoidosis
Symptoms and signs-
1. Neck Swelling
Lymph node character
i) Stone hard: typical of cancer usually metastatic
ii) Firm rubbery: can suggest lymphoma
iii) Soft: infection or inflammation
iv) Matting: tubercular
2. Pain-
(i) Painful lymph node present in acute inflammatory condition.
(ii) Painless lymph node mainly present in granulomatous or malignant conditions
3. Size - Rapid increase in size could be due to malignancy.
Evaluation-
1. Laboratory studies
a) CBC count, including a careful evaluation of the peripheral blood smear.An erythrocyte sedimentation rate is nonspecific but may be helpful.
b) Evaluation of hepatic and renal function and a urine analysis are useful to identify underlying systemic disorders that may be associated with lymphadenopathy.
c) Additional studies, such as lactate dehydrogenase (LDH), uric acid, calcium, and phosphate, may be indicated if malignancy is suspected. Skin testing for tuberculosis is usually indicated.
d) In evaluating specific regional adenopathy, lymph node aspirate for culture may be important if lymphadenitis is clinically suspected.
e) Titers for specific microorganisms may be indicated, particularly if generalized adenopathy is present. These may include Epstein-Barr virus, cytomegalovirus (CMV), Toxoplasma species, and human immunodeficiency virus (HIV).
2. Imaging studies
a) Chest radiography is usually the primary screening imaging study. Additional imaging studies are usually based on abnormal chest radiograph findings. Chest radiography is often helpful in elucidating mediastinal adenopathy and underlying diseases affecting the lungs, including tuberculosis, coccidioidomycosis, lymphomas.
b) CT scan and MRI especially helpful in case of metastatic disease to knowthe extent of involvement.
c) Nuclear medicine scanning is helpful in the evaluation of lymphomas.
d) Ultrasonography may be helpful in evaluating the changes in the lymph nodes and in evaluating the extent of lymph node involvement in patients with lymphadenopathy.
3. Fine Needle aspiration Cytology
4. Lymph Node Biopsy / Excisional Biopsy
Management-
1. Treatment with antibiotics (covering the bacterial pathogens frequently implicated in lymphadenitis) followed by re-evaluation in 2-4 weeks is reasonable if clinical findings suggest lymphadenitis. Benign reactive adenopathy may be safely observed for months.
Infectious lymph adenopathy usually requires treatment with appropriate antibiotics.
2. Granulomatous condition requires an address of general condition and treatment with steroids and immunoglobins depending on conditions.
3. In cases of malignant conditions, a patient can be managed on the different modality of treatment viz chemotherapy, radiotherapy or surgery depending on the type and stage of malignancy.
The above guideline has been developed by the Ministry of Health & Family Welfare, Govt. of India with Group Head Coordinator of Development Team as Dr J M Hans Ex-HOD Dept. of Otorhinolaryngology Dr.RML Hospital New Delhi
Medical Dialogues Bureau consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


