- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
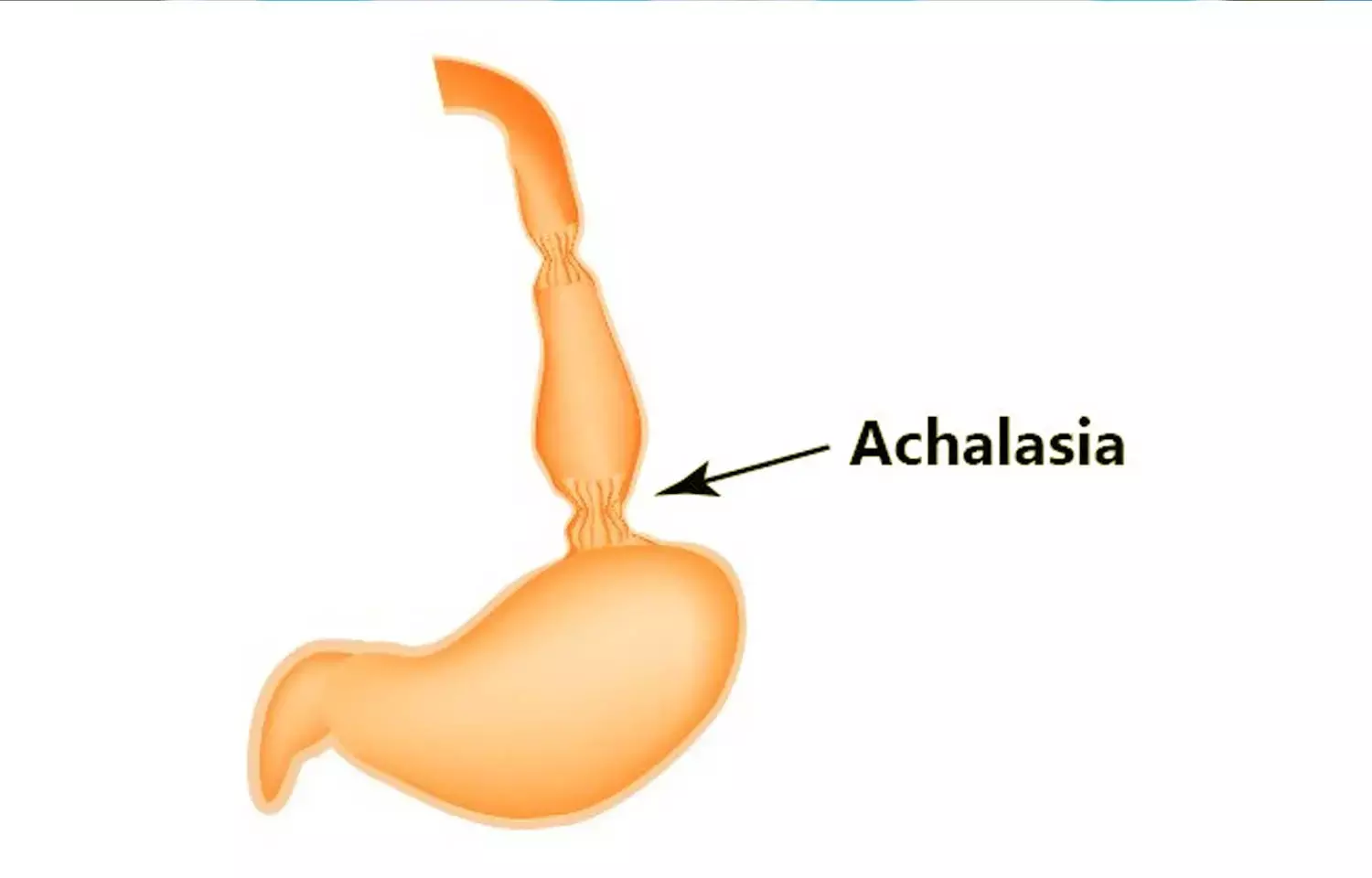
ACG releases Guidelines for Management of Achalasia
Recently the American College of Gastroenterology has published new guidelines for the diagnosis, treatment, and overall management of adult patients with Achalasia. The study was published in the journal "The American Journal of Gastroenterology" 2020.
Achalasia is one of the most studied esophageal motility disorders. It is characterized by aberrant peristalsis and insufficient relaxation of the lower esophageal sphincter. The most common symptoms are dysphagia to solids and liquids, regurgitation, and occasional chest pain with or without weight loss. The American College of Gastroenterology has proposed few guidelines for the diagnosis and the management of adults with Achalasia. They used the Grading of Recommendations Assessment, Development, and Evaluation process to provide clinical guidance on how best to diagnose and treat patients with achalasia. The guideline is structured in the format of recommendations, key concepts, and summaries of the evidence.
Some of the recommendations are as follows:
• Patients who are initially suspected of having Gastroesophageal reflux disease (GERD) but do not respond to acid-suppressive therapy should be evaluated for achalasia.
• They recommended esophageal pressure topography over conventional line tracing for the diagnosis of achalasia.
• They suggested that classifying achalasia subtypes by the Chicago Classification may help inform both prognosis and treatment choice.
• They recommended botulinum toxin injection as first-line therapy for patients with achalasia that are unfit for definitive therapies.
• They recommended that treatment with botulinum toxin injection does not significantly affect the performance and outcomes of the myotomy.
• They did not suggest obtaining routine gastrograffin esophagram after dilation due to a lack of evidence.
• They recommended that myotomy with fundoplication is superior to myotomy without fundoplication in controlling distal esophageal acid exposure.
• They suggest either Dor or Toupet fundoplication to control esophageal acid exposure in patients with achalasia undergoing surgical myotomy.
• They recommended tailored POEM or laparoscopic Heller myotomy (LHM) for type III achalasia as a more efficacious disruptive therapy of the lower esophageal sphincter (LES) compared with Pneumatic dilation(PD).
• They supported the evidence that in patients with achalasia, POEM compared with LHM with fundoplication or PD is associated with a higher incidence of GERD.
• They recommended esophagectomy in surgically-fit patients with megaesophagus who have failed other interventions.
• They recommended against stent placement for the management of long-term dysphagia in patients with achalasia despite low-quality data.
• They recommended that PD is superior to medical therapy in relieving symptoms and physiologic parameters of esophageal emptying.
• They recommended that PD or LHM are both effective and equivalent short- and long-term procedures for patients with achalasia who are candidates to undergo definitive therapy.
• They recommended that POEM or PD result in comparable symptomatic improvement in patients with types I or II achalasia.
• They recommended that POEM and LHM result in comparable symptomatic improvement in patients with achalasia.
They concluded by recommending that Eckardt score (ES) or high-resolution manometry (HRM) alone not be used to define treatment failure. Hence recommend using Timed Barium esophagram (TBE) as the first-line test in evaluating continued or recurrent symptoms after definitive therapy for achalasia.
For further reading, click the following link: doi: 10.14309/ajg.0000000000000731
BDS, MDS
Dr.Niharika Harsha B (BDS,MDS) completed her BDS from Govt Dental College, Hyderabad and MDS from Dr.NTR University of health sciences(Now Kaloji Rao University). She has 4 years of private dental practice and worked for 2 years as Consultant Oral Radiologist at a Dental Imaging Centre in Hyderabad. She worked as Research Assistant and scientific writer in the development of Oral Anti cancer screening device with her seniors. She has a deep intriguing wish in writing highly engaging, captivating and informative medical content for a wider audience. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


