- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
PPIs interfere with achievement of remission in IBS patients on infliximab: Study
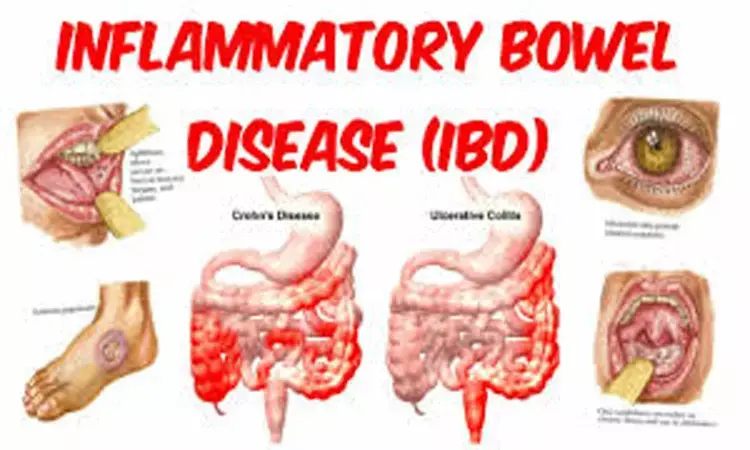
It has been recently observed that patients with inflammatory bowel disease (IBD) taking proton pump inhibitors (PPI) are less likely to achieve remission while on infliximab therapy, according to recent research published in The Gut.
In treating patients with inflammatory bowel disease (IBD), how concomitant medications influence the response to infliximab is largely unexplored. Therefore, Thomas X Lu and associates from the Inflammatory Bowel Disease Center, University of Chicago Medicine, Chicago, USA carried out this study to evaluate whether proton pump inhibitors (PPIs) affect the response to infliximab therapy in patients with IBD.
Patient-level data of adult patients with moderate-to-severe IBD treated with infliximab were obtained from the Yale Open Data Access Framework. Multivariable analysis and propensity score-matched analysis were performed to assess week 30 remission rates, week 54 remission rates and hospitalisation rates in patients on infliximab therapy with and without PPI exposure.
The authors included a total of 889 patients and 147 patients on infliximab with and without PPI therapy, respectively. Patients on PPI were older, more likely to be Caucasian and were less likely to be on immunomodulator therapy.
The key findings of the study revealed-
a. Patients on PPI were significantly less likely to achieve week 30 remission on multivariable analysis (OR 0.45, p<0.001).
b. Following propensity score matching adjusting for baseline difference in patient characteristics, the week 30 remission rates were 30% and 49% in patients with and without PPI therapy, respectively (p<0.001).
c. Analyzing separately for disease, the findings remained statistically significant in Crohn's disease but did not reach significance in UC. Similar results were seen with week 54 remission rates.
d. Patients on PPI were also more likely to be hospitalised (15% vs 8%, p=0.007).
e. Rates of adverse events such as gastroenteritis were not different between the two groups.
Hence, the authors concluded that "patients with IBD taking PPI were less likely to achieve remission while on infliximab therapy."
The results of the study warrant further investigation into the effect of PPI on IBD outcomes and therapies, they further added.
Dr. Nandita Mohan is a practicing pediatric dentist with more than 5 years of clinical work experience. Along with this, she is equally interested in keeping herself up to date about the latest developments in the field of medicine and dentistry which is the driving force for her to be in association with Medical Dialogues. She also has her name attached with many publications; both national and international. She has pursued her BDS from Rajiv Gandhi University of Health Sciences, Bangalore and later went to enter her dream specialty (MDS) in the Department of Pedodontics and Preventive Dentistry from Pt. B.D. Sharma University of Health Sciences. Through all the years of experience, her core interest in learning something new has never stopped. She can be contacted at editorial@medicaldialogues.in. Contact no. 011-43720751
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


