- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
New Wilderness Medical Society guidelines may help reduce tick-borne illness
Philadelphia The number of cases of tick-borne illnesses (TBIs) reported annually to the Centers for Disease Control and Prevention (CDC) has more than doubled over the past two decades in the United States.
An expert panel has developed a set of clinical practice guidelines that recommends low-risk interventions, employable with minimal resources, to help reduce the number of TBIs. The guidelines, issued by the Wilderness Medical Society, appear in Wilderness & Environmental Medicine, published by Elsevier.
Although Lyme disease is the most commonly reported vector-borne disease in the United States, the incidence of other TBIs, including anaplasmosis, spotted fever rickettsiosis, babesiosis, tularemia, alpha-gal syndrome, and Powassan virus, continues to rise as well. Lyme disease accounted for nearly 70% of cases of TBI reported in 2019, anaplasmosis 16%, and spotted fever rickettsiosis 10%. Experts believe that formal reporting probably underestimates the disease burden.
"TBI is influenced by the environment, geography, climate, ecology, and animal and human behavior," explained lead author Benjamin M. Ho, MD, Southern Wisconsin Emergency Associates, Janesville, WI, USA. "It cannot be completely avoided given the interactions between humans and the environment. However, the overall burden of disease related to TBIs can be reduced with certain behavioral and medical adaptations."
The Wilderness Medical Society convened an expert panel to develop evidence-based guidelines for the prevention and management of TBI. The guidelines include a brief review of the clinical presentation, epidemiology, prevention, and management of TBIs in the United States, with a primary focus on interventions that are appropriate for resource-limited settings. Their recommendations are largely consistent with those presented by the CDC and other practice guidelines, but they specifically highlight concepts most relevant to providers who encounter ticks in backcountry, austere, and limited-resource settings.
Clinical practice guidelines include:
Wear long-sleeved clothing when traveling in tick habitat.
Light-colored clothing may not reduce the risk of tick bites but makes it easier to identify ticks on clothes during tick checks.
N-diethyl-meta-toluamide (DEET) is an effective tick repellent. It can be used in children over the age of two months.
- The efficacy of picaridin compares favorably to DEET. It may have a superior safety profile when compared to DEET.
- Permethrin-treated clothing may further reduce the risk of TBI when used in combination with a skin-based tick repellent such as DEET or picaridin.
- Avoid essential oils, citriodiol, nootkatone, and IR3535 as a first line repellent as they have either a lower repellent efficacy or significantly shorter duration of action.
- Evidence supporting tick checks is contradictory but may help prevent TBI when combined with showering or bathing within two hours of returning from tick habitat.
- Washing clothes at temperatures over 54°C/130°F and drying clothing in high heat for ten minutes kills ticks and may reduce the risk of TBIs.
- When feasible, avoid areas with high grass or leaf litter. When in tick habitat, walk in the middle of trails to reduce the chance of contact with ticks.
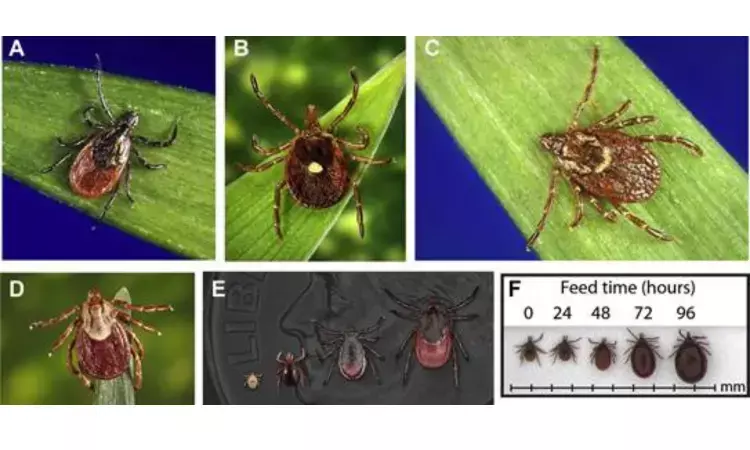
- Mechanical removal by pulling upward, or perpendicular to skin with forceps, directly on an embedded tick, is the best currently available method. Commercial devices may also work, but there is no evidence suggesting they are superior. Pulling embedded ticks with straight, steady pressure is preferred over a twisting movement.
- Chemical strategies that involve exposing attached ticks to petroleum jelly, fingernail polish, isopropyl alcohol, gasoline, or methylated spirits are ineffective and not recommended.
- There is no evidence that using local or systemic medications such as locally infiltrated anesthetics or systemic ivermectin is effective in removing or exterminating attached ticks.
- Remove ticks as soon as possible. To meaningfully reduce the risk of Lyme disease, ticks should be removed within 36 hours.
- A single dose of 200 mg doxycycline orally is recommended after a high-risk tick bite to reduce the risk of Lyme disease if given within 72 hours.
- Outside of high-risk Lyme disease exposures, prophylactic antibiotics are not indicated.
- Individuals who develop systemic or high-risk symptoms (fever, generalized rash, arthralgias, cranial nerve palsy, dyspnea, or syncope) related to a suspected TBI should be evacuated to a higher level of medical care.
- Individuals who develop symptoms suggestive of Lyme carditis such as dyspnea, dizziness, or syncope should receive a screening ECG as soon as possible and would benefit from a thorough cardiovascular evaluation in an appropriate clinical setting.
- Although no vaccine for tick-borne encephalitis is currently available in the United States, vaccines such as Encepur appear to be efficacious for inducing seroconversion against tick-borne encephalitis.
- Educational programs should be encouraged as these can change behavior and lower rates of TBI.
"With a changing climate that continues to influence the epidemiology of TBI, promotion and strict adherence to simple prevention measures is important," commented Dr. Ho. "Despite the limitations of the existing literature, these guidelines provide a starting point for front-line providers to mitigate the transmission and reduce the disease burden of TBIs through education and low-risk interventions."
Hina Zahid Joined Medical Dialogue in 2017 with a passion to work as a Reporter. She coordinates with various national and international journals and association and covers all the stories related to Medical guidelines, Medical Journals, rare medical surgeries as well as all the updates in the medical field. Email: editorial@medicaldialogues.in. Contact no. 011-43720751
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


