- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Vitamin D, fish oil supplements don't lower atrial fibrillation risk: JAMA
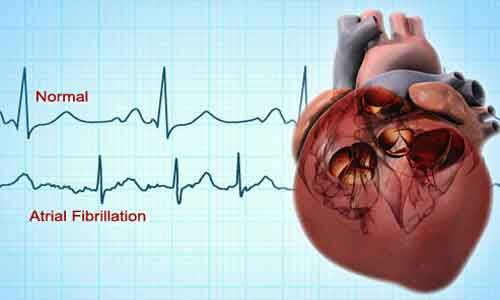
USA: Supplementation with marine omega-3 fatty acids or vitamin D does not significantly impact atrial fibrillation (AF) risk compared to placebo in adults aged 50 years or older, finds a recent study.
The findings of the study, published in the journal JAMA, do not support the use of vitamin D3 or marine omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) for the prevention of atrial fibrillation.
In their analysis, Albert and her research team also examined whether vitamin D or omega-3 fatty acids might have an impact on paroxysmal versus persistent atrial fibrillation and whether there might be certain subgroups of patients who would be more likely to benefit or be harmed by the supplements. Overall, the results were mostly consistent across types of AF and groups of patients.
"The incidence of atrial fibrillation (AF), the most common heart rhythm disturbance, continues to increase, and results in significant mortality and morbidity," wrote the authors. "The marine omega-3 fatty acids, EPA and DHA, and vitamin D have been shown to have both risks and benefit with respect to incident AF, but there is a lack of large-scale, long-term randomized trial data."
To fill this knowledge gap, Christine M. Albert, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, California, and colleagues aimed to test the effects of long-term administration of marine omega-3 fatty acids and vitamin D on incident AF.
For the purpose, the researchers conducted an ancillary study of a 2 × 2 factorial randomized clinical trial involving 25 119 women and men aged 50 years or older without prior cardiovascular disease, cancer, or AF. Participants were recruited directly by mail between November 2011 and March 2014 from all 50 US states and were followed up until December 31, 2017.
Among the 25 119 participants who were randomized and included in the analysis, 24 127 (96.1%) completed the trial.
The participants were randomized to receive EPA-DHA (460 mg/d of EPA and 380 mg/d of DHA) and vitamin D3 (2000 IU/d) (n = 6272 analyzed); EPA-DHA and placebo (n = 6270 analyzed); vitamin D3 and placebo (n = 6281 analyzed); or 2 placebos (n = 6296 analyzed).
Key findings of the study include:
- Over a median 5.3 years of treatment and follow-up, the primary end point of incident AF occurred in 900 participants (3.6% of study population).
- For the EPA-DHA vs placebo comparison, incident AF events occurred in 469 (3.7%) vs 431 (3.4%) participants, respectively (hazard ratio, 1.09).
- For the vitamin D3 vs placebo comparison, incident AF events occurred in 469 (3.7%) vs 431 (3.4%) participants, respectively (hazard ratio, 1.09).
- There was no evidence for interaction between the 2 study agents.
"Among adults aged 50 years or older, treatment with EPA-DHA or vitamin D3, compared with placebo, resulted in no significant difference in the risk of incident AF over a median follow-up of more than 5 years," concluded the authors. "The findings do not support the use of either agent for the primary prevention of incident AF."
Reference:
The study titled, "Effect of Marine Omega-3 Fatty Acid and Vitamin D Supplementation on Incident Atrial Fibrillation: A Randomized Clinical Trial," is published in the journal JAMA.
DOI: https://jamanetwork.com/journals/jama/fullarticle/2777469
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


