- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Kidney transplant recipients recovering from COVID-19: Management strategies, outcomes
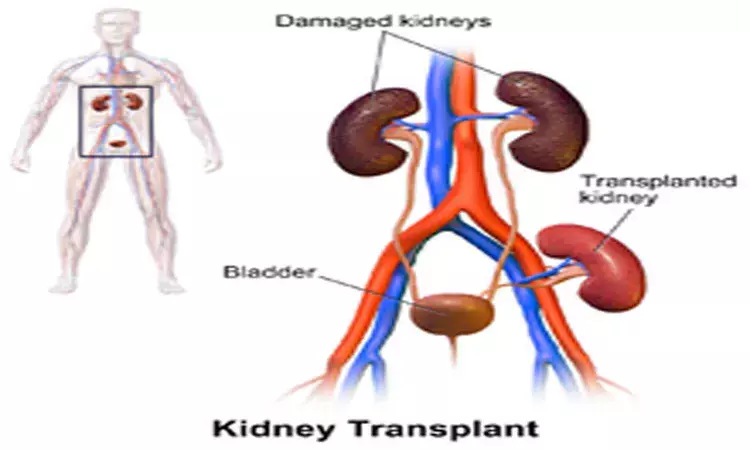
The outcomes of Kidney transplant (KT) after COVID-19 recovery are excellent with the absence of COVID-19 sequelae during follow-up and there does not seem to be a need for changes in the induction/immunosuppression regimen based on the severity of COVID-19, a study has found. The study has been published in eClinicalMedicine.
 Also Read:Decoding REGEN-COV2 for Mild to Moderate SARS-CoV-2 Infection in Kidney Transplant Recipients
Also Read:Decoding REGEN-COV2 for Mild to Moderate SARS-CoV-2 Infection in Kidney Transplant Recipients
There is an enormous knowledge gap in management strategies, clinical outcomes, and follow-up after kidney transplantation (KT) in recipients that have recovered from coronavirus disease (COVID-19). The study was a multicentre, retrospective, cohort study that was conducted at transplant centers across India between June 26, 2020 (the index transplant date of the study) to December 1, 2021 (the last follow-up date). Through a nationwide collaboration of 23 participating centers, data of a total of 372 KT in COVID-19 recovered patients were collected.
Among 372 KT which included 38(10·21%) ABO-incompatible, 12(3·22%) sensitized 64(17·20%) coexisting donors with COVID-19 history, and 20 (5·37%) recipients with residual radiographic abnormalities, the incidence of AR was 34 (9·1%) with 1(0·26%) death censored graft loss, and 4(1·07%) all-cause mortality over a median (interquartile range) follow-up of 241 (106–350) days. In our cox hazard proportional analysis, the absence of oxygen requirement during COVID-19 compared to oxygen need [HR = 0·14(0·03–0·59); p-value = 0·0071], and use of thyroglobulin use compared to other induction strategies [HR = 0·17(0·03–0.95); p-value = 0·044] had a lower risk for AR. Degree of Human leukocyte antigen (HLA) DR mismatch had the highest risk of AR [HR = 10.2(1·74–65·83); p-value = 0·011]. With competing risk analysis, with death as a competing event, HLA DR mismatch, and oxygen requirement continued to be associated with AR. Age, gender, obesity, inflammatory markers, dialysis vintage, steroid use, sensitization, and ABO-incompatibility have not been associated with a higher risk of AR. The median duration between COVID-19 real-time polymerase test negativity to transplant was 88(40–145) days (overall), and ranged from 88(40–137), 65(42–120), 110(49–190), and 127(64–161) days in World Health Organization ordinal scale ≤ 3, 4, 5, and 6–7, respectively. There was no difference in the quality of life, tacrolimus levels, blood counts, and mean serum creatinine assessed in patients with a past COVID-19 infection independent of the severity.
Patients with severe clinical COVID-19 symptoms requiring oxygen or those with a less potent induction treatment had more frequent acute rejection (AR) in the report. This observation can be explained by the fact that the patients with increasing COVID-19 severity, who are well known to have greater co-morbidities, had a trend for a lower induction strategy. Based on the findings, we hypothesize that COVID-19 disease severity or recovery time may not serve as a criterion for reducing immunosuppression.
The strength of this study is based on an extensive and detailed follow-up, a large number of 100(27%) moderate-severe cases, feasibility and safety of transplants in 20(5·37%) recipients with residual radiological abnormality in the chest without active infection before transplant surgery, 38(10·21%) ABO-incompatible KT, 12(3·22%) sensitized patients, and 64(17·20%) donor/recipient pairs who recovered from COVID-19. We tested and demonstrated that the outcomes in the above-mentioned high-risk transplantation are also safe while yielding favorable graft outcomes.
 Also Read:Mineralocorticoid receptor antagonists improve outcomes in kidney failure patients on dialysis
Also Read:Mineralocorticoid receptor antagonists improve outcomes in kidney failure patients on dialysis
MBBS
She is passionate about writing and loves to read, analyses and write informative medical content for readers. She can be contacted at editorial@medicaldialogues.in. Contact no. 011-43720751
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


