- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Rare case of Miller Fisher syndrome: a report
Dr Karan N. Ramakrishna at Department of Medicine, State University of New York (SUNY) Upstate Medical University, NY, USA and colleagues have reported a rare case of Miller Fisher syndrome. The case has appeared in the Journal of Medical Case Reports.
Miller Fisher syndrome is a variant of acute inflammatory demyelinating polyneuropathy classically characterized by ataxia, ophthalmoplegia, and areflexia. Miller Fisher syndrome can present with uncommon symptoms such as bulbar, facial, and somatic muscle palsies and micturition disturbance.
According to history, a 76-year-old white man presented to the emergency department (ED) with a recent onset of unsteady gait, poor oral intake, dysarthria, and dizziness for 1 week prior to presentation. His wife called an ambulance and had him brought to our ED as she noticed he was short of breath for the prior 12 hours. He did not have any symptoms suggestive of a recent upper respiratory tract infection or gastroenteritis. He denied exposure to sick contacts, recent immunizations, or consumption of canned foods or beverages. He did have a past medical history significant for oesophagal stricture (diagnosed 2 years before) for which he had been undergoing routine endoscopic balloon dilation (the last attempt was 3 months before). He lived in a rural upstate New York county and had retired as a meat-cutter 15 years before. His only medications at the time were ferrous sulfate (324 mg daily), pantoprazole (40 mg twice daily), and a multivitamin. He did not have a history of tobacco smoking. He consumed approximately two standard drinks in a week. He had no known allergies. While in our ED, his vital signs were: temperature, 37 ºC (98.6 ºF); heart rate, 100–110 beats per minute; blood pressure, 141/82 mmHg; and oxygen saturation 82% on room air and requiring 100% fraction of inspired oxygen (FiO2) via facemask to maintain saturations above 96%. On physical examination, he was in marked respiratory distress but not toxic-appearing. He was awake but drowsy, oriented only to self. His pupils were equal and symmetrical with appropriate response to light. His extraocular movements were intact. There was no facial droop; there was no deviation of tongue or uvula. His gag reflex was impaired. He could move all four extremities spontaneously and on command. However, motor strength appeared to be symmetrically and mildly diminished in all extremities and accompanied by a decreased tone. Diminished knee and ankle reflexes were noted bilaterally. He had a diminished flexor plantar response bilaterally. The sensation was grossly intact in his face, trunk, and extremities. Coordination was impaired in the upper and lower extremities with dysmetria and dysdiadochokinesia. Gait was not assessed. He had no visible involuntary movements. His neck was supple without signs of meningismus. A cardiovascular examination was unremarkable, with normal heart sounds and equal symmetrical pulses in bilateral extremities. His abdominal, musculoskeletal, and skin examinations were unremarkable. Although he was hemodynamically stable, he became lethargic with stridor and progressive hypoxia. Given concern for airway protection, he was emergently intubated with a 7.5 mm endotracheal tube on first attempt and placed on mechanical ventilatory support. For intubation, he was administered 1.5 mg/kg of succinylcholine and 0.3 mg/kg of etomidate intravenously. Maintenance fluids (normal saline at 125 cc/hour) and empiric intravenous administration of ceftriaxone at a dose of 2 g every 24 hours (to cover for possible aspiration pneumonia) was initiated. He was transferred to our intensive care unit for further management. A nasopharyngolaryngoscopy revealed bilateral true vocal cord paralysis. After stabilization on a ventilator, he underwent a tracheostomy on day 3 of admission and was transitioned successfully to a tracheostomy collar. Following extubation, he had consistent and gradual recovery of mental status. This was not, however, accompanied by any progressive improvement in motor function. He continued to have vocal cord immobility and flaccid weakness of his extremities.
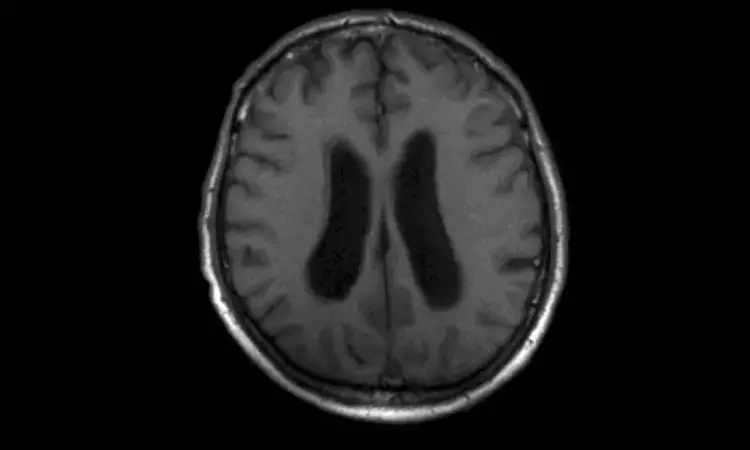
On presentation, laboratory testing revealed a white blood cell (WBC) count, 13,800 cells/μL; hemoglobin, 14.7 g/dl; platelet count, 235,000 cells/μL; sodium, of 143 mmol/L; potassium, 4.2 mmol/L; chloride, 105 mmol/L; glucose, 176 mg/dL; bicarbonate, 27 mmol/L; creatinine, 0.53 mg/dL; blood urea nitrogen (BUN), 15 mg/dL; and calcium, 8.0 mg/dL. A hepatic function panel revealed a total protein level, 5.2 g/dL; serum albumin, 3.5 g/dL; total bilirubin, 0.5 mg/dl; aspartate aminotransferase (AST), 18 U/L; alanine aminotransferase (ALT), 21 U/L; international normalized ratio (INR), 1.08; creatine kinase, 127 U/L; and troponin I less than 0.015 ng/mL. Urine analysis demonstrated cloudy urine with specific gravity 1.018, pH 4.8, with 116 red blood cells (RBCs) and 4 white blood cells (WBCs), negative leukocyte esterase and nitrite. An electrocardiogram and chest X-ray were unremarkable. A urine drug screen and serum alcohol levels were negative. Serum thyroid-stimulating hormone (TSH) and cortisol levels were within normal limits. Thiamine, vitamin B6, and B12 levels were normal. Serological tests were negative for Lyme disease, human immunodeficiency virus (HIV), syphilis, hepatitis B, and hepatitis C. Blood and urine cultures obtained at presentation showed no growth. Non-contrast computed tomography (CT) of his head and magnetic resonance imaging (MRI) of his brain were normal except for mild ventriculomegaly. CT angiography of his head and neck revealed patent intracranial vasculature. A repetitive nerve stimulation electromyographic (EMG) study demonstrated patchy, moderate to severe, peripheral motor nerve denervation consistent with AIDP. A lumbar puncture was performed and analysis of the obtained cerebrospinal fluid (CSF) showed albuminocytologic dissociation with less than 3 nucleated cells per mL of fluid, elevated CSF protein of 62 mg/dl, and normal glucose levels (88 mg/dl). CSF cultures did not demonstrate any growth. Anti-GQ1B antibody and anti-acetylcholine receptor (AChR) antibody levels were negative.
Based on the above, a diagnosis of MFS involving the bulbar muscles was made and our patient was started on a 5-day course of intravenous immunoglobulin at a daily dose of 0.4 mg/kg body weight per day. Following completion of this course, he showed clinical improvement in phonation, overall muscle strength, as well as tone. Although he initially did require overnight ventilatory support through his tracheostomy, the need for this gradually diminished and he was weaned off the ventilator altogether.
Subsequent follow-up laryngoscopies after 1, 2, and 4 weeks showed improvement in vocal cord abduction. His overall respiratory status also improved with decreasing oxygen requirement and decreased need for tracheostomy suctioning. He continued to have moderate pharyngeal dysphagia and required placement of a jejunostomy tube for feeding. His hospitalization was also complicated with the development of aspiration pneumonia. He was eventually discharged to a skilled nursing facility on a tracheostomy collar and jejunostomy tube after a total of 6 weeks of hospitalization and subsequently discharged home after making suitable progress in physical rehabilitation. He continued to follow-up with the physical medicine and rehabilitation (PMR) out-patient clinic and remained tracheostomy-dependent at 6 months following hospitalization. He was able to ambulate with a walker at that time.
For further reference log on to :
Hina Zahid Joined Medical Dialogue in 2017 with a passion to work as a Reporter. She coordinates with various national and international journals and association and covers all the stories related to Medical guidelines, Medical Journals, rare medical surgeries as well as all the updates in the medical field. Email: editorial@medicaldialogues.in. Contact no. 011-43720751
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


