- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Ectopic pregnancy: Risk factors, clinical presentation and management
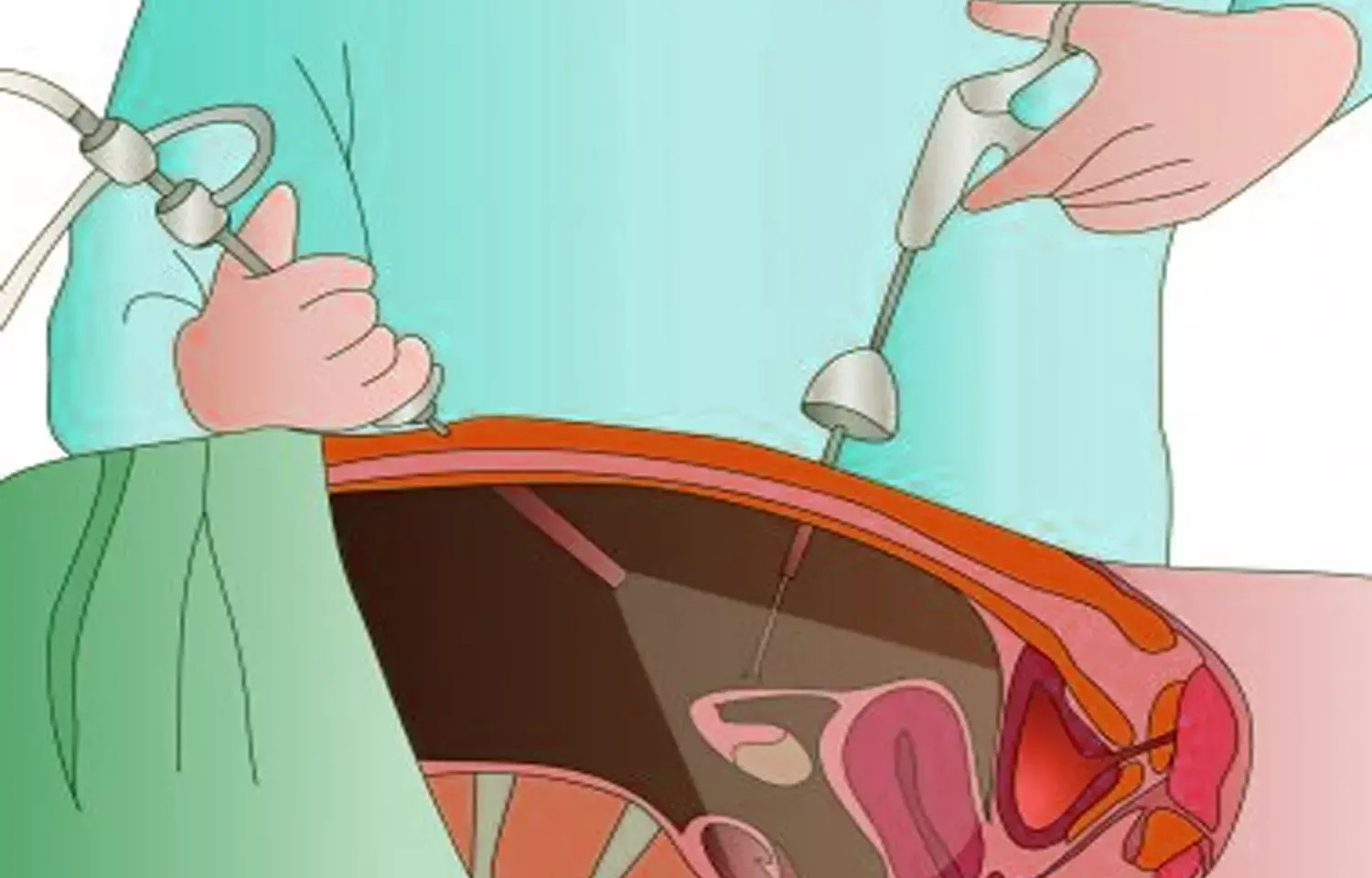
Implantation of a fertilised ovum outside the normal uterine cavity is called ectopic pregnancy. Of all the recognised pregnancies, the incidence of ectopic pregnancy is 2% approximately. Fallopian tube is the most commonest location for ectopic pregnancy (95%). In Fallopian tube, most common site is the ampulla, followed by isthmus, infundibulum and interstitium. Other less common sites are abdomen, ovary and cervix.
Ectopic pregnancy is the most common life threatening emergency which can lead to maternal death. Increase in incidence of pelvic inflammatory disease, smoking in reproductive age group women, previous abdominal surgeries and the use of assisted reproductive techniques are the various risk factors for ectopic pregnancy.
The clinical triad of ectopic pregnancy includes amenorrhoea, abdominal pain and bleeding per vagina. Other symptoms include haemorrhagic shock, passage of fleshy casts, fever and vomiting. The early diagnosis of ectopic pregnancy is due to improvement in non invasive techniques like transvaginal sonography and pregnancy tests in urine and serum. The clinical presentation of ectopic pregnancy has changed from life threatening disease requiring emergency surgery to a benign condition and in asymptomatic women nonsurgical treatment options are available now.
As ectopic pregnancy has variable presentations from asymptomatic to life threatening conditions, the aim of this study carried out by Saketha, John and Rathod was to determine the risk factors, clinical presentations and study the management modalities and outcome, so as to make recommendations on interventions to reduce the morbidity of this condition.
This was an observational study of 90 cases of ectopic pregnancies admitted to the Department of Obstetrics and Gynaecology at a tertiary care teaching hospital from February 2019 to August 2020. Relevant data of the 90 patients was tabulated and descriptive analysis was done. Patients with positive urine pregnancy test without any intrauterine gestational sac were diagnosed as ectopic pregnancy based on USG features of adnexal mass and/or intraperitoneal free fluid suggestive of haemoperitoneum and were included in the study.
Parameters like age, blood group, parity, history of previous ectopic pregnancy, previous abdominal surgery, history of dilatation and curettage, pelvic inflammatory disease, usage of intrauterine device were studied. Symptoms like bleeding per vagina, amenorrhea, pain abdomen and shock were studied.
Majority of the patients belonged to 21-30 yrs age group. Maximum number of cases (57%) had a history of previous abdomino pelvic surgery. The predominant symptom was amenorrhea (96.6%) and classical triad of amenorrhea, bleeding per vagina and abdominal pain was seen in 30% of the study population. Majority of the patients i.e 76.7% underwent surgical intervention.
Risk factors:
- Previous abdominal surgery 57.7%
- Spontaneous abortion 10%
- ART 10%
- Infertility 8.8%
- Previous ectopic pregnancy 4.4%
- Dilatation and curettage 7.7%
- TB 2.2%
Symptoms:
- Amenorrhea 96.6%
- Pain abdomen 81.1%
- Bleeding pv 58.8%
- Syncope 7.7%
- Vomiting 22.2%
- Passage of clots 10%
- Fever, Shoulder tip pain
Signs:
- Abdominal tenderness 54.4%
- Fullness in fornix
- Tenderness in fornix 36.6%
- Adnexal mass, Abdominal distension, Abdominal mass
- Cervical motion tenderness 25.5%
USG findings:
- Free fluid in POD 71.1%
- Adnexal mass 50%
- Gestational sac 18.8%
- Cardiac activity 4.4%
Among patients who presented with ectopic gestation, majority belonged to the age group of 21-30 years (71.1%). Regarding risk factors, history of previous abdominal surgery was the most important one i.e 52 cases (57.7%). Amenorrhea was the most common symptom and abdominal tenderness the commonest sign being present in 96.6% and 54.4% patients respectively. Free fluid in pouch of Douglas was the commonest finding (71.1%) in ultrasonogram. Surgical intervention was the main mode of management in 69(76.7%) patients since majority presented with ruptured ectopic with haemoperitoneum 42(46.7%). Medical management with methotrexate was successful in 84.6% cases (11 out of 13 cases) and expectant management in 8 cases.
The Study gives an idea of the necessary symptoms and signs to keep a watch for in case of diagnosed ectopic pregnancy with the risk factors and management to reduce morbidity and mortality associated with the diagnosis.
Source: Saketha, John and Rathod / Indian Journal of Obstetrics and Gynecology Research 2021;8(3):296–300
MBBS, MD Obstetrics and Gynecology
Dr Nirali Kapoor has completed her MBBS from GMC Jamnagar and MD Obstetrics and Gynecology from AIIMS Rishikesh. She underwent training in trauma/emergency medicine non academic residency in AIIMS Delhi for an year after her MBBS. Post her MD, she has joined in a Multispeciality hospital in Amritsar. She is actively involved in cases concerning fetal medicine, infertility and minimal invasive procedures as well as research activities involved around the fields of interest.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


