- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Model predicts number of MII oocytes needed to obtain at least one euploid blastocyst: Study
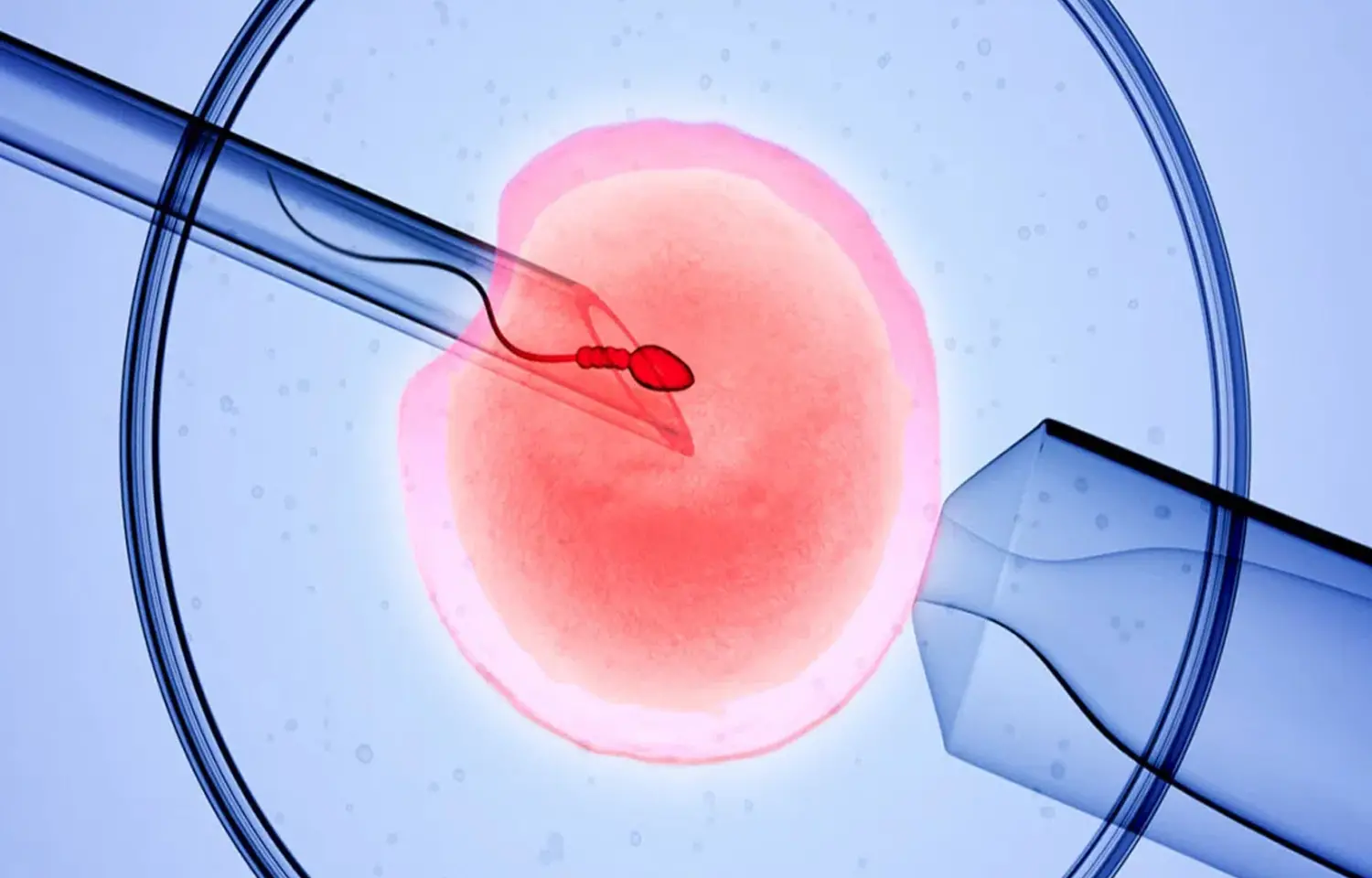
Female age is significantly and directly related to embryo aneuploidy rates. The current delay in motherhood has led to a large proportion of women of advanced maternal age seeking infertility treatment, thus presenting significantly higher embryo aneuploidy rates. Consequently, these patients are characterized by lower chances of success in in vitro fertilization (IVF) treatments with their own oocytes and many of them are finally encouraged to enter the oocyte donation program.
In the assumption of the statement ‘‘the older the patient, the lower the number of euploid blastocysts,’’ there is a frequently asked question in the day-to-day operations of an infertility clinic: how many oocytes each of our patients’ needs, according to female age, to have the highest chances of obtaining at least one euploid blastocyst in their IVF treatment cycles? The answer to this question would constitute useful information for both the clinician and the patient. On the one hand, the clinician may be able to better assess each patient’s possibilities and the feasibility of their treatment cycle because it will be easier to explain the patient’s options. On the other hand, the patient will understand this information more easily, helping her to cope emotionally with treatment. This is nowadays feasible because predicting ovarian response with high precision before starting treatment has become possible with the use of novel biomarkers, such as antimullerian hormone levels and/or antral follicle count.
The aim of the present study by Cristina Rodríguez-Varela et al was to design a similar tool to determine the number of metaphase II (MII) oocytes needed to obtain at least one euploid blastocyst regarding female age in IVF treatment cycles, considering our own data from the last 5 years using next-generation sequencing (NGS) on TE biopsies. This information will help to decide the best strategy for each patient and her individual situation.
Eligible patients were undergoing their first IVF-PGT-A treatment cycle, in which at least one MII oocyte was obtained, regardless of oocyte and semen origin. Oocyte donation cycles were included in the donor group (≤34 years old). Treatment cycles from women with their own oocytes were selected only when the oocytes were aged ≥35 years (patient group). Only trophoectoderm biopsies performed on days 5 or 6 of development and analyzed using next-generation sequencing were included. Preimplantational genetic testing for aneuploidy cycles because of a known abnormal karyotype were excluded.
A total of 2,660 IVF-PGT-A treatment cycles were performed in the study period in the eligible population (patients group = 2,462; donors group =198). The mean number of MII oocytes needed to obtain one euploid blastocyst increased with age, as did the number of treatment cycles that did not get at least one euploid blastocyst. An adjusted multivariate binary regression model was designed using 80% of the patient group sample (n = 2,462; training set). A calculator for the probability of obtaining at least one euploid blastocyst was created using this model. The validation of this model in the remaining 20% of the patient group sample (n = 493; validation set) showed that it could estimate the event of having at least one euploid blastocyst with an accuracy of 72.0%
The minimum number of MII oocytes needed to have high chances of obtaining at least one euploid blastocyst increases with increasing maternal age. Study model estimates with an accuracy of 74% the probability of having at least one euploid blastocyst, considering oocyte age and the number of MII oocytes. This model has been created with the largest database of IVF-PGT-A treatment cycles ever used for this purpose, including only PGT-A treatment cycles using NGS on TE biopsies. Once this model has been validated prospectively and in multicenter studies, it may be useful for both the clinician and the patient coming to an infertility clinic, whether or not a PGT-A analysis is performed. The clinician may use this data to propose the best strategy for each patient, whereas the patient may use this information to better understand the likelihood of obtaining an euploid blastocyst, helping her to cope emotionally with IVF treatment. Nevertheless, to this day, this model has limited clinical value. It should be further validated and optimized to use it as a clinical support tool, in our own clinic and in many others.
Source: Cristina Rodríguez-Varela, M.Sc.,a Juan Manuel Mascaros, M.Sc., a Elena Labarta; Fertil Steril® Vol. 122, No. 4, October 2024 https://doi.org/10.1016/j.fertnstert.2
MBBS, MD Obstetrics and Gynecology
Dr Nirali Kapoor has completed her MBBS from GMC Jamnagar and MD Obstetrics and Gynecology from AIIMS Rishikesh. She underwent training in trauma/emergency medicine non academic residency in AIIMS Delhi for an year after her MBBS. Post her MD, she has joined in a Multispeciality hospital in Amritsar. She is actively involved in cases concerning fetal medicine, infertility and minimal invasive procedures as well as research activities involved around the fields of interest.


