- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Multiplexed serum biomarkers may help discriminate nonviable and ectopic pregnancy: Study
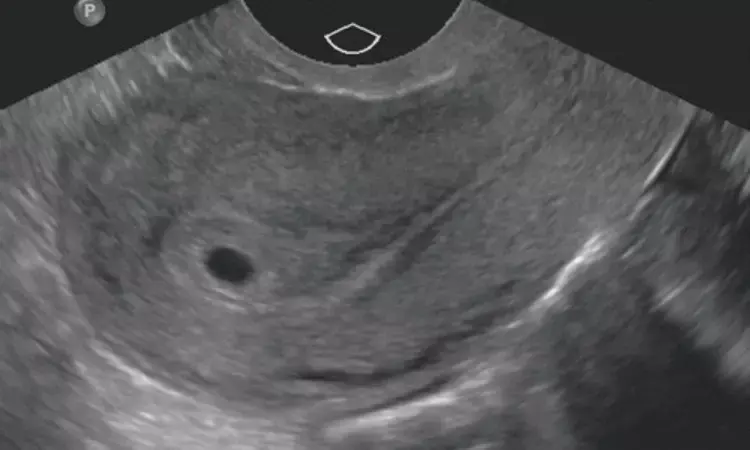
For decades, the standard of care for early pregnancy assessment has been transvaginal ultrasound (TVUS) and serum human chorionic gonadotropin (hCG) levels. An accurate diagnosis of live intrauterine pregnancy (IUP), early pregnancy loss (EPL), or ectopic pregnancy (EP) can be made in most individuals at initial presentation. However, a definitive diagnosis often cannot be made early in gestation when a normal IUP is not expected to be visualized using ultrasound or when normal ultrasound milestones are not present. Even when gestational age is advanced enough to use ultrasound as a diagnostic test, approximately 20%–40% of individuals will not have a definitive diagnosis and are at risk of having a nonviable pregnancy (EP or EPL). The standard of care for follow-up is serial hCG levels, but this approach also has limitations and can misclassify.
The successful identification and application of biomarkers produced during early pregnancy could change the diagnostic standard, providing an earlier diagnosis or useful information when ultrasound is not diagnostic. Biomarkers could be useful before TVUS visualization of a pregnancy or when TVUS is not definitive.
The development of a companion diagnostic on the basis of biomarkers is an iterative process. Authors first evaluated biomarkers suggested in the literature to have biological plausibility to predict early pregnancy outcomes in a series of case-control experiments. After establishing and validating candidates with acceptable assay performance and discriminatory capacity individually, they sought to further improve predictive capacity by assessing them in combination. In this study, they assessed the most promising 24 markers and used multiple machine learning (ML)-based methodologies to evaluate combinations of these top candidates to develop a multiplexed prediction model for the identification of a nonviable pregnancy and an EP.
A nested case-control design evaluated the predictive ability and discrimination of biomarkers in patients at risk of early pregnancy failure in the first trimester to classify viability and location. A total of 218 individuals with pain and/or bleeding in early pregnancy: 75 had an ongoing intrauterine gestation; 68 had ectopic pregnancies (EPs); and 75 had miscarriages. Serum levels of 24 biomarkers were assessed in the same patients. Multiple machine learning-based methodologies to evaluate combinations of these top candidates to develop a multiplexed prediction model for the identification of a nonviable pregnancy (ongoing intrauterine pregnancy vs. miscarriage or EP) and an EP (EP vs. ongoing intrauterine pregnancy or miscarriage). The predicted classification using each model was compared with the actual diagnosis, and sensitivity, specificity, positive predictive value, negative predictive value, conclusive classification, and accuracy were calculated.
Models using classification regression tree analysis using 3 (pregnancy-specific beta-1-glycoprotein 3 [PSG3], chorionic gonadotropin-alpha subunit, and pregnancy-associated plasma protein-A) biomarkers were able to predict a maximum sensitivity of 93.3% and a maximum specificity of 98.6%. The model with the highest accuracy was 97.4% (with 70.2% receiving classification). Models using an overlapping group of 3 (soluble fms-like tyrosine kinase-1, PSG3, and tissue factor pathway inhibitor 2) biomarkers achieved a maximum sensitivity of 98.5% and a maximum specificity of 95.3%. The model with the highest accuracy was 94.4% (with 65.6% receiving classification). When the models were used simultaneously, the conclusive classification increased to 72.7% with an accuracy of 95.9%. The predictive ability of the biomarkers in the random forest produced similar test characteristics when using 11 predictive biomarkers.
Authors demonstrated that a small pool of biomarkers, used in combination, can be used to classify individuals with potential EPL as not viable and extra uterine. The overall test characteristics are modestly dependent on the number of biomarkers used. The biomarkers CG-alpha, PAPPA, and PSG3 can be used to predict viability and sFlT, TPFI2, and PSG3 can be used to predict pregnancy location.
Source: Fertil Steril® Vol. 122, No. 3, September 2024 https://doi.org/10.1016/j.fertnstert.2024.04.028
MBBS, MD Obstetrics and Gynecology
Dr Nirali Kapoor has completed her MBBS from GMC Jamnagar and MD Obstetrics and Gynecology from AIIMS Rishikesh. She underwent training in trauma/emergency medicine non academic residency in AIIMS Delhi for an year after her MBBS. Post her MD, she has joined in a Multispeciality hospital in Amritsar. She is actively involved in cases concerning fetal medicine, infertility and minimal invasive procedures as well as research activities involved around the fields of interest.


