- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
"Intravitreal Dexamethasone implant effective for postoperative macular oedema": Study
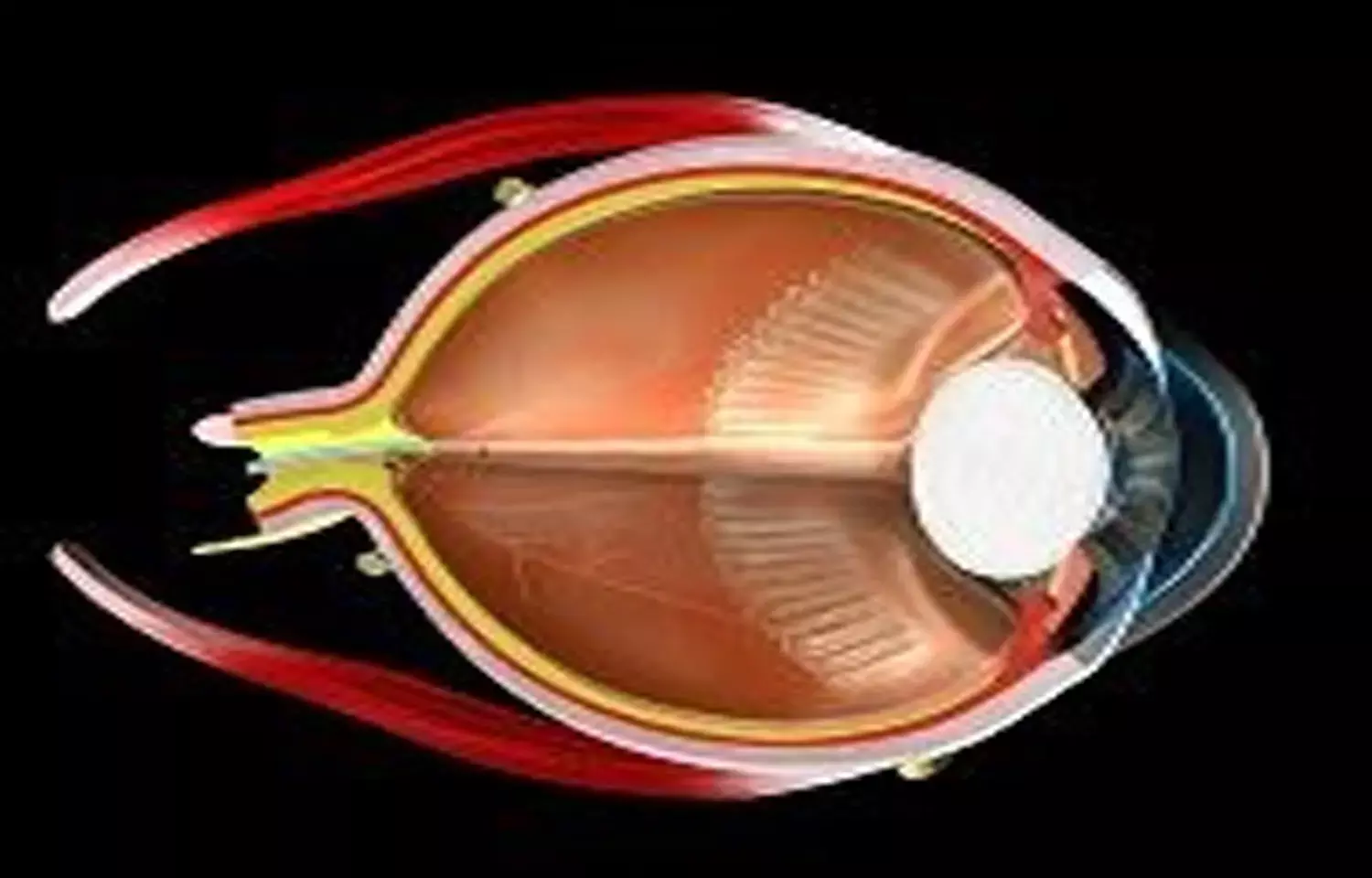
Postoperative cystoid macular oedema (CMO) represents one of the main causes of postoperative visual impairment, generally occurring between 4 and 12 weeks after surgery. This condition has been also reported following vitrectomy, with an incidence as high as 47% of cases. Its etiology mainly depends on an inflammatory process triggered by the surgery. For such a reason, steroids have been widely used for the treatment of postoperative CME, including the sustained release dexamethasone intravitreal implant (DEX).
Guglielmo Parisi et al systematically reviewed the scientific evidence on the intravitreal dexamethasone implant (DEX) for the treatment of macular oedema secondary to vitrectomy for epiretinal membrane (ERM) and retinal detachment (RD) and performed meta-analyses on visual and anatomical outcomes. The study was published in Journal of Ophthalmology, Hindawi publication.
Studies reporting clinical outcomes of DEX use for the treatment of macular oedema secondary to ERM and RD vitrectomy were searched on PubMed and Embase databases. The primary outcome was best-corrected visual acuity (BCVA) change between baseline and post-DEX treatment, reported as mean difference (MD) with 95% confidence interval (CI). Mean central macular thickness (CMT) change was assessed as a secondary outcome. Postimplant adverse events, including intraocular pressure rise and cataract development, were reported as well.
Five uncontrolled studies, 1 nonrandomized controlled study, and 1 randomized controlled study were included, with a total of 5 cohorts and 3 cohorts in the ERM group and RD group, respectively. Considering the last available follow-up, a significant improvement in postimplant BCVA was found in the overall population, irrespective of the indication for vitrectomy but with significant heterogeneity. In either group, mean BCVA significantly improved following the implant with no difference between the two groups.
Considering the last available follow-up, a significant CMT reduction was found in the overall population, irrespective of the indication for vitrectomy . In the ERM group, a significant CMT reduction was shown following DEX ,with no heterogeneity. In the RD group, mean CMT reduction was borderline significant with significant heterogeneity. No difference in CMT improvement was found between the two groups
The present meta-analysis showed favorable visual and anatomical outcomes following the use of dexamethasone implant for macular oedema secondary to ERM and RRD vitrectomy.
Postvitrectomy macular oedema is a sight-threatening condition which could affect visual recovery following a successful surgery. This complication has been reported in roughly 15% of cases following RRD vitrectomy, while its incidence ranges from 13% to 47% following ERM vitrectomy.
The causative mechanisms of postvitrectomy macular oedema have not been completely understood yet. It seems that inflammation plays a key role in this process. Indeed, macular oedema following RRD vitrectomy has been associated with the presence of proliferative vitreoretinopathy (PVR) and with longstanding RRD, which, in both cases, are likely to be linked with an inflammatory status . Furthermore, macula-off RRD has been associated with a higher rate of postvitrectomy macular oedema. In case of ERM vitrectomy, macular distortion due to the contractile membrane has been assumed to trigger the inflammatory condition.
In the above context, the use of the intravitreal 0.7 mg dexamethasone implant is being investigated. DEX is characterized by a potent anti-inflammatory activity and a good safety profile. A remarkable advantage of the slow release implant is its efficacy in vitrectomized eyes, which are less suitable to intravitreal antivascular endothelial growth factor (antiVEGF) therapy because of a faster washout.
"When considering the last available follow-up, our analyses revealed a significant visual gain following DEX administration in both the ERM and the RRD groups, and in the overall population as well. Similarly, a significant reduction in macular thickness was shown in the overall population. Such an anatomical improvement was evident in the ERM group, while it was borderline significant in the RRD group due to a wide confidence interval."
When considering the different follow-ups, significant visual and anatomical improvements were demonstrated in both groups at 1 and 6 months. At 12 months, significant visual and anatomical improvements were shown in the ERM group, while these were nonsignificant in the RRD group.
Most of the included studies reported on persistent postvitrectomy macular oedema, which proved unresponsive to topical nonsteroidal anti-inflammatory drugs (NSAIDs) and/or periocular or intravitreal triamcinolone acetonide.
Chronic postsurgical macular oedema is unlikely to resolve spontaneously and its treatment might prove challenging. The fact that DEX provided both a functional and anatomical improvement in vitrectomized eyes with, in most cases, persistent CMO is worth noting, in particular taking into account that a low number of implants (from 1 to 1.7) was administered over a follow-up ranging from 3 to 12 months. In this systematic review, DEX-related adverse events were collected as well.
In general, the main adverse events related to dexamethasone implant were IOP rise and cataract. Most eyes of the included studies were pseudophakic at the time of DEX implant. This could be explained by the fact that these eyes had undergone a previous vitrectomy and cataract surgery could have been performed at that time or before.
Limitations of the study included significant heterogeneity for BCVA analysis in both groups and for CMT analysis in the RRD group. The presence of high heterogeneity limits the quality of the evidence provided. Additionally, no analysis was conducted on potential adverse events, such as IOP rise and cataract, due to the limited number of cases reported. Finally, a relatively small number of studies was included. However, a metaanalysis is featured by a greater power and accurate confidence interval compared with an individual study.
The researchers concluded , "The use of intravitreal dexamethasone implant for macular oedema following vitrectomy for ERM and RRD allowed improving both visual and anatomical outcomes. The implant represents a valid therapeutic option for this sight-threatening condition."
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


