- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Air tamponade may reduce ocular hypertension risk During Vitrectomy for Rhegmatogenous Retinal Detachment
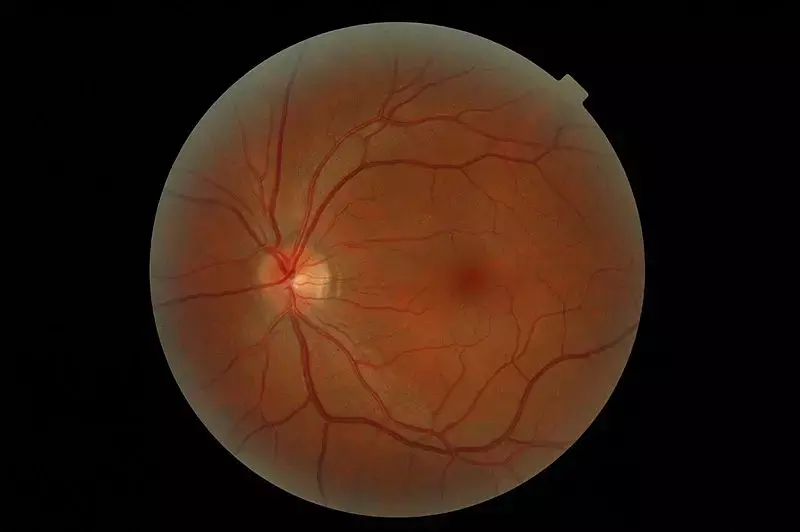
Rhegmatogenous retinal detachment (RRD) is a serious retinal disorder that can lead to blindness. The best treatment technique has been debated by ophthalmologists. Because RRD treatment had changed continuously, these changes need to be frequently evaluated. Several studies have reported an increase in the uses of pars plana vitrectomy (PPV) for treating eyes with RRD
However, PPV for RRD treatment has some disadvantages, including limitations in its day-to-day use due to gas tamponade. Typically, long-acting gases (LAGs), such as sulfur hexafluoride (SF6) and octafluoropropane (C3F8), have been chosen for tamponade. However, several studies have demonstrated the effectiveness of room air tamponade for RRD treatment for reducing patient discomfort. Although air tamponade has advantages, such as early discharge, surgeons are sometimes hesitant to use it due to the lack of patient selection criteria.
The choice of tamponade for RD should be individualized based on the location and characteristics of RD, expected patient compliance with postoperative positioning requirements, and other factors. Nakamura et al considered that it is easy for surgeons to select air tamponade for cases with RD that is relatively mildly severe. Moreover, they created an air tamponade selection criterion. The purpose of this study was to investigate the proper use of tamponade by comparing the effectiveness of both air tamponade and SF6 gas tamponade during vitrectomy for treating RRD in our proposed criteria.
Authors reviewed 294 eyes with RRD treated with 25-gauge vitrectomy by a single surgeon between June 2011 and April 2018 retrospectively. The exclusion criteria for the proposed air tamponade selection were more than 2 weeks since onset, giant retinal tears, history of complications following cataract surgery, high myopia, and proliferative vitreoretinopathy classified as grade C or higher. They examined the differences in the therapeutic effect between the air group and SF6 group at 6-month follow-up.
A total of 294 eyes were included in the study, 156 eyes in the air group and 138 eyes in the SF6 group. No difference was observed in the primary anatomical success rates between the air group and the SF6 group ( P = 0.102). Postoperative intraocular gas half-life was shorter in the air group (3.97 ± 0.87 days) compared with that in the SF6 group (8.67 ± 1.47 days P = 0.0001). The incidence of postoperative ocular hypertension was lower in the air group (19.9%) than in the SF6 group (62.3% P = 0.0001).
In the tamponade selection for general RD, LAGs, including SF6/C3F8 and silicone oil, are commonly chosen for severe cases and inferior break. Advances in vitreous surgery have resulted in attempts to select air tamponade over LAG for repositioning the retina as well as alleviating patient discomfort
In the air tamponade selection criteria proposed in this study, including less than 2 weeks since onset, air tamponade and SF6 gas tamponade had the same therapeutic effects.
In this study, authors were able to verify in detail that elevated IOP is a complication of air tamponade or SF6 gas tamponade. Generally, it is believed that tamponade with room air has a lower probability of increased IOP compared with LAGs, such as SF6 and C3F8. This study also revealed that the incidence of postoperative ocular hypertension was lower in the air group. Although LAG is advantageous for the treatment of RRD due to long-term filling in the eye, study demonstrated once again that it was disadvantageous to the air tamponade for increasing IOP. Postoperative ocular hypertension was observed not only the day after surgery but also several days after. Ocular hypertension was transitory and treated only with anti-glaucoma eye drops. It is an important clinical point to note that in this study, the use of tamponade in the eye caused an increase in IOP of about 20% in air and about 60% in SF6. The results of this study indicate that the risk of increased IOP can be greatly reduced by selecting air.
The half-life of the tamponade was about 4 days in the air and approximately 8 days for the SF6 gas. The results suggest that the half-life of air and SF6 was long because vitreous shaving was performed as much as possible and the three ports were sutured in all cases to prevent eye collapse. The results of longer half-life of air and SF6 may also be due to the fact that all the eyes in this study had phacoemulsification of the lens; therefore lens removal increased the volume of space to hold the air or gas. In this study, regardless of the location of the retinal breaks or the state of RD, the patients maintained the prone position until the intraocular gas concentration was reduced in half by the uniform half-life. In addition, the nurse continually checked the patient's position during hospitalization. Based on the criteria of this study, the therapeutic effect is sufficient when the prone position is continued for about 4 days. Even if the patient does not know whether he or she can properly maintain a prone position during surgery, it is necessary to verify whether the air tamponade is effective.
In summary, authors proposed the criteria for properly selecting between air tamponade or SF6 gas tamponade during vitrectomy for the treatment of RRD. They found no differences in the therapeutic effect exhibited by air tamponade and SF6 gas tamponade based on the proposed selection criteria for air tamponade. Furthermore, the incidence of elevated IOP was lower with air tamponade than with SF6 gas tamponade. Future prospective studies should be conducted to verify the therapeutic effect of air tamponade.
Source: Nakamura et al; Clinical Ophthalmology 2022:16 981–986
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


