- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Bilateral single orbital triamcinolone injections provided relief from Thyroid Eye Disease symptoms, reveals research
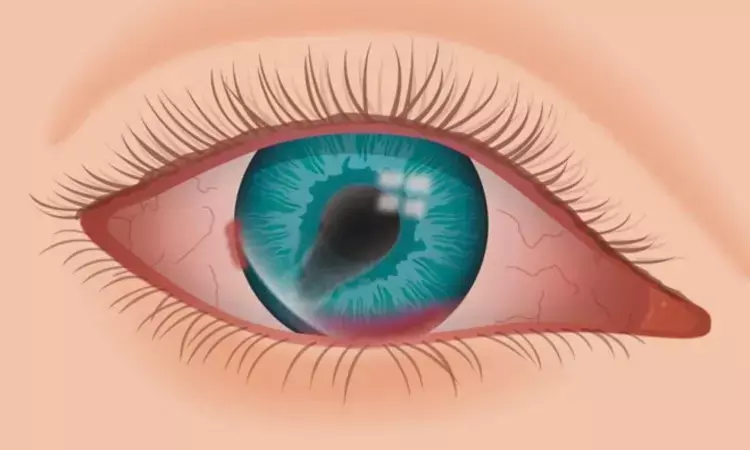
Thyroid eye disease (TED) represents a prevalent type of orbital tissue inflammation associated with autoimmune disorders linked to thyroid dysfunction, which is characterized by a spectrum of metabolic and immunologic disturbances. Because of their potent anti-inflammatory and immunosuppressive properties, systemic glucocorticoids have traditionally served as the first-line treatment for TED to mitigate inflammation. However, their use is fraught with a plethora of adverse effects, encompassing hyperglycemia, hypertension, metabolic disorders leading to the characteristic “moon face”, gastric ulcers, osteoporosis, and an increased susceptibility to infectious diseases.
To circumvent these adverse effects, local administration of glucocorticoids has been explored. Localized delivery is accomplished through subconjunctival, and sub-Tenon injections. In contrast, retro-orbital-septal injection offers an alternative method. This procedure, performed transcutaneously using a half-inch, 27-G needle, facilitates the precise delivery of medication into the lateral lower deep orbital fat, yielding promising results in the anti-inflammatory treatment of orbital tissue.7 Furthermore, Bagheri et al reported retroorbital-septal injection of triamcinolone and dexamethasone into both the upper and lower quadrants of the orbital soft tissue.
In this report, this approach was applied for patients with active TED who were resistant to or dependent on systemic steroids or faced complications related to systemic steroid use. The results demonstrated a significant reduction in orbital inflammation, including upper and lower eyelid retraction, ocular motility issues, and inflammatory markers such as the Clinical Activity Score (CAS) and NOSPECS classification. An intriguing aspect of the retro-orbital-septal delivery method is its capacity to produce a dramatic effect after only one or two injections.
Thus, this novel procedure may have advantages not only in local control of orbital inflammation but also in mitigating systemic adverse effects. However, no study to date has comprehensively evaluated the systemic effects of orbital corticosteroid injections, primarily because of the systemic absorption of the medication. The current report aimed to address this gap by focusing on the efficacy and systemic effects of deep orbital injection of triamcinolone, with the intent of promoting and advancing this procedure. To achieve this goal, authors conducted a prospective clinical investigation involving TED patients who underwent a single deep orbital injection of triamcinolone, followed by comprehensive ophthalmic and pharmacological assessments, including blood and urinary panels.
In a prospective investigation conducted from January 2021 to March 2023, patients diagnosed with TED were enrolled. Inclusion criteria encompassed a Clinical Activity Score (CAS) of ≥3, extraocular muscle inflammation, and upper eyelid retraction. A total of 1 mL of triamcinolone acetonide (40 mg/mL) was administered posterior to the orbital septum at both the medial and lateral aspects of both the upper and lower eyelids. Parameters, including CAS, margin-reflex distances (MRD1 and MRD2), intraocular pressure (IOP), ocular motility (Hess area ratio [HAR%]), exophthalmometry, extraocular muscle size, and blood and urinary indices, were evaluated before and at 2 and 4 weeks after a single injection.
Analysis included 28 patients (23 women, 5 men; mean age (SD): 38.7 (11.1) years), representing 56 eyes. Following the injection at 4 weeks, the mean CAS and MRD1 significantly decreased by 2 points and 0.8 mm, respectively. There was a 4.5% increase in HAR%, and extraocular muscle size decreased by 4 to 15.3 mm². Neutrophil count, C-reactive protein, and thyroid antibodies significantly decreased. No severe adverse ophthalmic or systemic effects, including IOP increases or liver damage, were observed.
In summary, this study robustly demonstrates the favorable effects of a single deep orbital corticosteroid administration for TED treatment without inducing substantial local or systemic adverse effects. Improvements in local and systemic assessments, TED-related antibody levels, and orbital muscle dimensions underscore the effectiveness of this intervention in modulating TED activity. While the study has limitations, including a limited patient cohort and a lack of iterative treatments, comprehensive validation will necessitate an expanded and iteratively treated patient series in the future.
Source: Yamana et al; Clinical Ophthalmology 2024:18 https://doi.org/10.2147/OPTH.S476562
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.


