- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Cultured Human Corneal Endothelial Cell Injection therapy provide rapid recovery of corneal endothelial failure
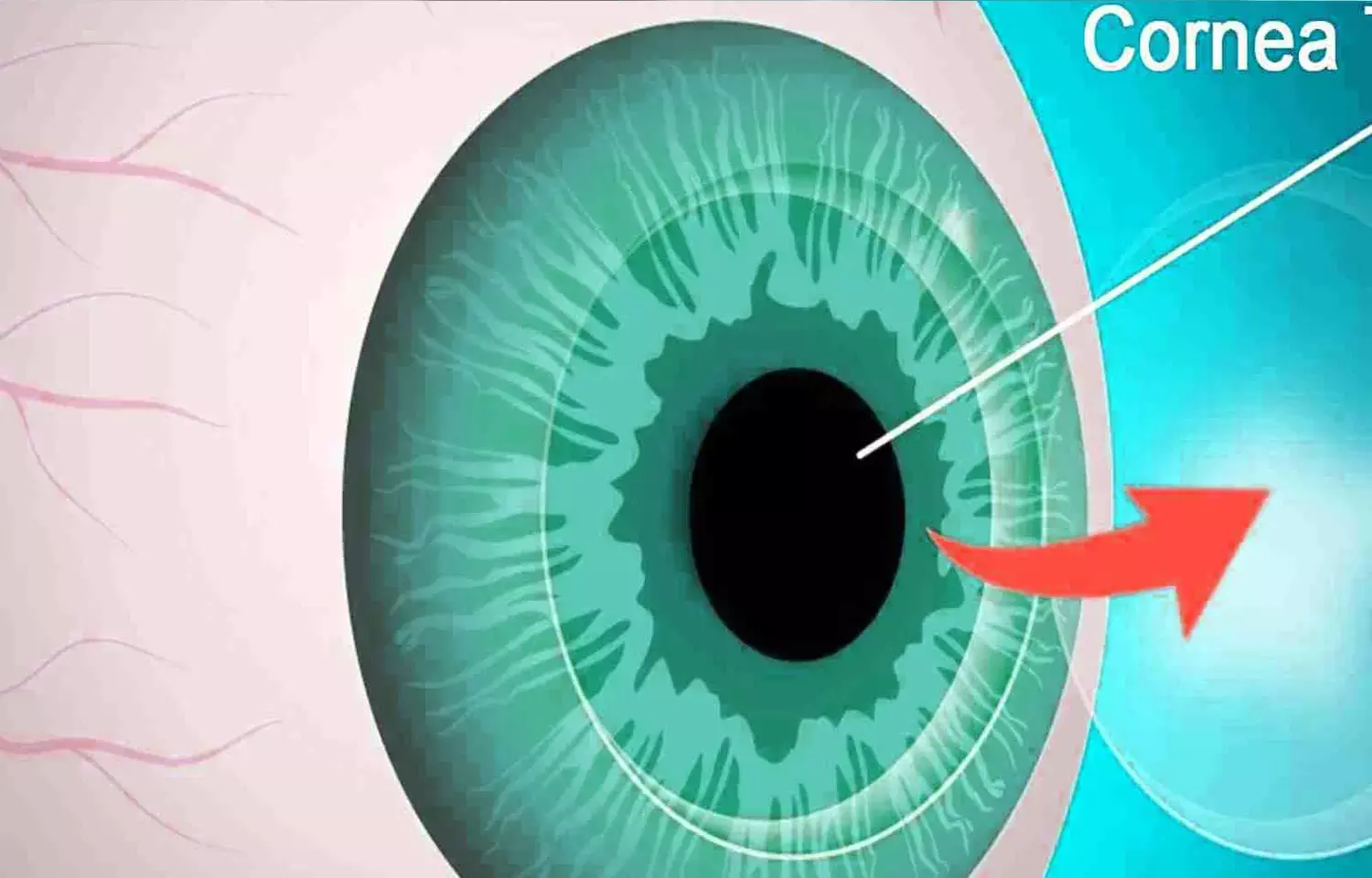
Currently, the treatments for moderate corneal endothelial dysfunction and corneal endothelial failure (CEF), classically termed "bullous keratopathy", include Descemet stripping automated endothelial keratoplasty (DSAEK), Descemet membrane endothelial keratoplasty (DMEK) and penetrating keratoplasty, all of which require the use of a fresh donor cornea.
The postoperative outcomes of DSAEK and DMEK are quite well known. However, for mild corneal endothelial dysfunction, such as Stage 1 or Stage 2 Fuchs endothelial corneal dystrophy (FECD), Descemet membrane stripping only (DSO), a surgical procedure that involves the removal of a small central corneal area of the Descemet membrane with guttae and degenerated endothelium, has been proposed. The benefit of DSO is that it does not involve the use of donor corneal tissue, while the disadvantage is a relatively low corneal endothelial cell (CEC) density (CECD) postoperative. Moreover, the long-term efficacy of DSO has yet to be fully elucidated.
Ideally, for cases of corneal endothelial dysfunction or CEF, the optimal therapy would be a minimally invasive procedure that reconstructs the cornea with a high CECD of homeostatic ordered CECs, thus maintaining a normal healthy corneal structure for a long-term period post treatment. Morio Ueno et al previously reported their novel surgical procedure involving the injection of allogeneic cultured human CECs (hCECs) with a ROCK inhibitor into the anterior chamber, and 5-year postoperative results revealed that new cultured hCEC-injection therapy is safe and effective with reasonably good long-term outcomes.
In this present study, in order to investigate and verify the superiority of the clinical outcomes in CEF patients treated with cultured hCEC-injection therapy using highly purified mature cultured hCECs (Group 2; Gr2), authors organized and initiated a small case series clinical trial. Moreover, they analyzed the collective order of the cultured hCECs prior to injection, and at 24-weeks and 3-years postoperative via our previously reported newly-developed method. Thus, the purpose of this current interventional study was to present clinical findings on the safety and efficacy of the cultured hCEC-injection therapy using the highly purified mature cultured hCECs (Gr2 treated eyes) compared with the findings obtained using the previously-reported Gr1 cultured hCECs (Gr1 treated eyes).
This study involved 18 eyes with CEF that underwent cultured hCEC injection therapy, categorized into two groups:
1) 11 eyes administered a relatively lower proportion (0.1 to 76.3%) of mature cell SPs [Group 1 (Gr1)], and
2) 7 eyes administered a relatively higher proportion (>90%) of mature cell SPs [Group 2 (Gr2)].
From 1-week to 3-years postoperative, corneal endothelial cell (CEC) density (CECD), central corneal thickness (CCT), and best-corrected visual acuity (BCVA) were recorded, and the CEC parameters, spring constant was calculated. The proportion of mature SPs was evaluated by fluorescence-activated cell sorting analysis based on cell-surface markers.
At 3-years postoperative, corneal restoration with improved BCVA was attained in 10 of the 11 Gr1 eyes and all Gr2 eyes, the median CECD in Gr2 (3,083 cells/mm2; range, 2,182-4,417 cells/mm2 ) was higher than that in Gr1 (1,349 cells/mm2 ; range, 746-2,104 cells/mm2 ) (P < 0.001), and the spring constant verified the superiority of the mature cultured hCECs. From 24-weeks through 3-years postoperative, the median percentage of CECD decrease was 3.2% in Gr2 and 23.6% in Gr1 (P < 0.005). CCT recovery was prompt and constant in Gr2, while diverse in Gr1. No adverse events were observed.
The findings in this interventional study confirmed that although the number of cells injected into the anterior chamber and the surgical procedure and postoperative care was identical between the two groups, cell-injection therapy using Gr2 cultured hCECs resulted in a better corneal restoration in terms of CECD than that using Gr1 cultured hCECs at both 24-weeks and 3-years postoperative, thus indicating the superiority of the Gr2 cultured hCECs, both at the early and mid-term postoperative periods.
Comparison of the early postoperative period between the two groups revealed that Gr2 cultured hCECs produced a faster recovery of corneal thinning than Gr1 cultured hCECs, probably due to the rapid functional recovery for corneal dehydration (i.e., the pump and barrier function).
In conclusion, the findings in this study suggest that a higher biological quality of cultured hCECs acquired via maximum quality control of the cell-culture procedure for the production of cells for hCEC-injection therapy can improve the long-term clinical outcomes and help prevent late-stage CEF post surgery.
Source: Morio Ueno , Munetoyo Toda , Kohsaku Numa et al, Superiority of Mature Differentiated Cultured Human Corneal Endothelial Cell Injection Therapy for Corneal Endothelial Failure, American Journal of Ophthalmology (2021)
doi: https://doi.org/10.1016/j.ajo.2021.11.012
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


