- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Mucormycosis management made handy in covid era: New scoring System for Orbital Exenteration
Humans are exposed to Mucormycosis fungi on a routine basis but rarely suffered any disease as their virulence was very low. It mainly affects those who are immunocompromised with Diabetes Mellitus being the most common pre-disposing factor. The other pre-disposing diseases that may contribute to mucormycosis are prior steroid therapy.
However in covid era, this deadly fungus has caused an epidemic due to immunocompromising ability of covid 19 along with injudicious use of steroids for covid treatment.
The most common mode of spread of these fungi is through inhalation of fungal spores or conidia.Once these spores enter the tissues, they find their way into the blood vessels and get lodged there. This then induces an inflammatory reaction which leads to formation of a thrombus which enlarges in size and ultimately leads to compromised blood supply of the tissues and thence causes ischaemic necrosis. The necrosis is responsible for the blackening of the tissues which is characteristic of Mucormycosis.
Depending upon the site of entry of infection into the orbit and the structure involved, the first symptoms the patients experience are decreased vision and mono-muscular palsy leading to diplopia. Late features include complete blindness, chemosis/proptosis, total ophthalmoplegia and optic atrophy on ophthalmoscopy. Further spread intra-cranially may lead to headache, altered consciousness and death
Mucormycosis is rapidly progressive, angio-invasive, commonly fatal, opportunistic fungal infection. The most critical decision in the management of rhino-orbital mucormycosis is whether the orbit should be exenterated.The decision for exenteration often depends on the judgment of the treating otolaryngologist and the ophthalmologist.
This prompted Kshitij Shah and team to devise a scoring system which efficiently tracks the orbital involvement by the disease and also lay down the indications of orbital exenteration in rhino-orbito-cerebral mucormycosis published in Indian Journal of Otolaryngology and Head and Neck Surgery.
Aims of the study included
- To layout the indications of orbital exenteration in patients with rhino-orbito-cerebral mucormycosis.
- To devise a scoring system that predicts the stage at which the exenteration needs to be carried out.
A scoring system was devised by a team of experienced Otorhinolaryngologists and Ophthalmologists from prior experience in managing mucormycosis.
A total of 15 patients were included.
The scoring system was based on 3 main criteria, namely:
(1) clinical signs and symptoms.
(2) Direct and Indirect Ophthalmoscopy.
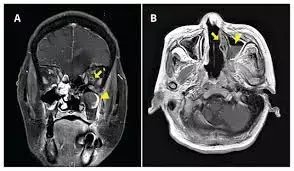
(3) Imaging
The scoring system was applied on the patients. Depending on the score, surgical debridement from the nasal/paranasal/oral region ± orbital exenteration was carried out within a period of 24–36 h of admission. Inj Amphotericin-B intravenously was started after an initial sensitivity test dose at strength of 1 mg/ kg/day and continued till a total dose of 2–3 g was completed.
A repeat nasal endoscopy was performed and tissue from the suspected diseased area was sent for microscopic examination on KOH mount. If KOH mount was found negative, Amphotericin-B was stopped. Patients were then discharged and followed up on OPD basis.
Based on the vision, salvage ability of the eye, likelihood of further spread and cosmesis, different number of points were given to different findings which are listed below
How the score was given:
1 point = Mild symptoms/signs
2 points = Moderate symptoms/signs
3 points = Severe symptoms/signs
A. Clinical
B. Opthalmology
C. Imaging
Based on the scoring system, it was observed that those patients who crossed a score of 23 were eligible candidates for orbital exenteration as agreed upon by the Otorhinolaryngologist and Ophthalmologists. It was found that most of these patients were in turn positive for mucormycoses on histopathology and are stable now after completion of Amphotericin therapy.
Table 1 Clinical symptoms
|
| 0 | 2 | 3 |
| Vision | Normal or same as prior to other symptoms | Decreased vision after developing other symptoms | Total blindness |
| Pupil | Normal | RAPD | Fixed |
| Ocular motility | Normal | Extra-ocular muscle palsy/Diplopia | Fixed eyeball |
| Proptosis | Absent | - | Present |
| Intracranial spread | Normal | Headache, projectile vomiting, confusion | Altered consciousness, Pulsatile Exophthalmos, coma |
Table 2 Ophthalmology
Fundus changes Points
Normal 0
Cotton wool spots 1
Congested tortuous retinal blood vessels 2
Optic disc oedema 2
Central retinal vein occlusion 2
Central retinal artery occlusion 2
Retinal detachment 2
Choroidal folds 2
Optic disc pallor 2
Total 15
Table 3 Imaging
Orbital involvement by the disease
(globe/muscles/fat) 3
Intracranial spread/superior orbital fissure/
inferior orbital fissure involvement 3
Optic neuritis 3
Sphenoid sinus involvement 2
Frontal sinus involvement 1
Ethmoidal sinus involvement 1
Infra-temporal fossa involvement 1
Maxillary sinus involvement 1
Management
- Surgical debridement of all the necrosed tissue along with Inj Amphotericin-B (1 mg/ kg/day for a total dose of 2–3 g) is the treatment of choice.
However, when the orbit is involved the decision making is not as direct. The vision is arguably the most important sensation of a human being. The decision to either preserve the eye or exenterate it as a part of surgical debridement has to be taken jointly by the otolaryngologists and the ophthalmologists.
- Orbital Exenteration with Enucleation
- Endoscopic Orbital Exenteration
- Amphotericin-B
- Orbital Reconstruction
The above comprise preferred management options for mucormycosis treatment. The decision has to be a close balance between preserving the eye or preventing further intra-cranial spread and eventually death.
New Management options include
- Posaconazole : It was given after 6 weeks of unresponsive Amphotericin-B treatment and there was significant clinical improvement as early as 7 days into the treatment with continued improvement for 23 weeks of therapy and no adverse reactions attributable to Posaconazole.
- HBO2 and G-CSF are the other medical management options that have shown some promise. They act by enhancing the leukocyte killing capacity and increase oxygen delivery to the tissues. Their role is however only additive to systemic anti-fungals.
The Sion Hospital Scoring System is an accurate and promising measure to solve the dilemma that is associated with orbital exenteration in orbito-rhino-cerebral mucormycosis. This scoring system devised by a team of experienced Otorhinolaryngologists and Ophthalmologists from prior experience in managing mucormycosis is now extensively being used to decide the line of management for the new encounter with epidemic of the disease in the covid era.
Source: Kshitij Shah, Varun Dave, Renuka Bradoo, Chhaya Shinde, M. Prathibha; Indian J Otolaryngol Head Neck Surg
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


