- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
NSAID monotherapy non inferior to steroid and NSAID combo for Cataract Surgery Prophylaxis: JAMA
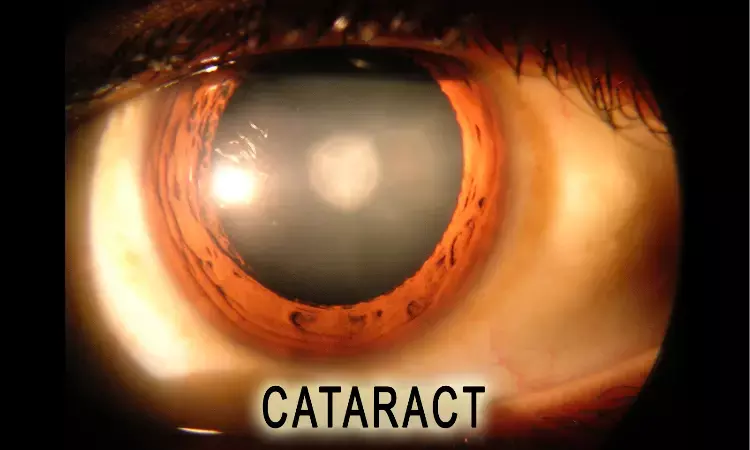
Pseudophakic cystoid macular edema (PCME) is an important cause of unsatisfactory visual outcome after cataract surgery. It affects visual acuity after approximately 1% of surgical procedures.
It is believed that PCME is caused by the inflammatory response after cataract surgery, which disrupts the blood ocular barrier leading to leakage of fluid into the retina. To control the inflammatory response and reduce the risk of PCME, prophylactic anti-inflammatory eye drops are prescribed parallel to cataract surgery.
The choice of anti-inflammatory prophylaxis is contested. Two types of drugs are available: corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs).Corticosteroids inhibit phospholipases and thereby both prostaglandin and lipoxin synthesis and NSAIDs selectively inhibit cyclooxygenase enzymes, which convert arachidonic acids to prostaglandins.
Prophylactic treatment parallel to cataract surgery is traditionally administered as eye drops. Many patients have difficulties using eye drops and need assistance. Therefore, several dropless approaches have been suggested, and some studies have found that the effectiveness of these dropless approaches is comparable to corticosteroid eye drop monotherapy.
The purpose of the study carried out by Jesper Erichsen and team was to determine whether
(1) combination of prednisolone and NSAID eye drops is superior in preventing macular thickening after uncomplicated cataract surgery compared with NSAID monotherapy and dropless surgery using a sub–Tenon capsule dexamethasone phosphate depot and
(2) Preoperative initiation of eye drop treatment is superior to initiating treatment on the day of surgery.
This investigator-driven, single-center, randomized clinical trial with masked statistical analyses enrolled patients at the Department of Ophthalmology, Rigs Hospitalet Glostrup, Glostrup, Denmark, from February 1, 2018, to August 15, 2019. Follow-up was completed December 18, 2019.
Participants included low-risk patients undergoing phacoemulsification for age-related cataract by an experienced surgeon (1 eye per participant). Data were analyzed from February 17 to June 15, 2020. Participants scheduled for cataract removal were randomized to 1 of 5 anti-inflammatory prophylactic regimens: eye drops with a combination of prednisolone, 1%, and ketorolac tromethamine, 0.5%, with or without preoperative initiation (preoperative prednisolone plus NSAID [control] and postoperative prednisolone plus NSAID groups), ketorolac monotherapy with or without preoperative initiation (preoperative and postoperative NSAID groups), or sub-Tenon depot of dexamethasone phosphate (sub-Tenon group). Eye drops were administered 3 times per day until 3 weeks postoperatively.
The primary outcome was central macular thickness at the 3-month visit measured by optical coherence tomography using the central 1.0-mm zone. Secondary outcomes were CST at 3 weeks postoperatively, corrected distance visual acuity (CDVA) in logarithm to the minimal angle of resolution (logMAR) using an ETDRS chart, intraocular pressure (IOP), and subjective tolerance of treatment.
A total of 470 participants with 94 participants in each group were included in the analysis.
Three months after surgery, the mean CST was 250.7 μm in the preoperative prednisolone plus NSAID group, 250.7 μm in the postoperative prednisolone plus NSAID group, 251.3 μm in the preoperative NSAID group, 249.2 μm in the postoperative NSAID group, and 255.2 μm in the sub-Tenon group. There were no significant differences in CST or visual acuity compared with control and no differences between preoperative and postoperative groups, but 47 of 83 participants (56.6%) in the sub-Tenon group needed additional anti-inflammatory treatment.
Authors found that NSAID plus corticosteroid drops were not superior to NSAID monotherapy or subTenon dexamethasone depot for postoperative central macular thickening after uncomplicated cataract surgery. One of the primary purposes of prescribing an antiinflammatory prophylactic treatment in parallel with cataract surgery is to prevent PCME. Pseudophakic cystoid macular edema is infrequent and heterogeneously defined, which makes it difficult to use the incidence as an outcome in clinical trials. Instead, the CST measured with optical coherence tomography is generally accepted as a measure for comparing efficacy of prophylactic regimens. Study did not find differences in CST between groups receiving NSAID monotherapy or a combination of NSAID and prednisolone
Preoperative initiation of therapy did not result in decreased CST compared with postoperative initiation, even after pooling relevant groups.
In the sub-Tenon group, CST was significantly increased 3 weeks postoperatively compared with the preoperative prednisolone plus NSAID group, but the difference was no longer significant 3 months after surgery. More than half of the participants in the sub-Tenon group required additional topical anti-inflammatory treatment during the study period, which might explain why no difference in CST was found at 3 months.
Intraocular pressure was lower during eye drop treatment in groups who did not use corticosteroid drops compared with those who did. However, the mean IOP in all groups was low in the reference range, and there were no elevations of greater than 25mm Hg at any postoperative visit. There were no differences in visual acuity at any time point, but adverse events and unscheduled visits were more often encountered in the sub-Tenon group.
In this randomized clinical trial, authors found that a combination of prednisolone and NSAID eye drops was not superior to NSAID monotherapy and that initiating prophylactic treatment 3 days before surgery was not superior to initiating treatment on the day of surgery in preventing thickening of the central subfield after uncomplicated cataract surgery.
In addition, they found that dropless surgery with a sub-Tenon dexamethasone depot was inferior to a combination of prednisolone and NSAID eye drops and that anti-inflammatory eye drops were required in a substantial number of participants in the sub-Tenon dexamethasone depot group. Intraocular pressure was higher in groups that used prednisolone eye drops compared with NSAID monotherapy and sub-Tenon dexamethasone depot in the first 3 weeks postoperatively. Therefore, NSAID monotherapy with initiation on the day of surgery may be preferred as an anti-inflammatory prophylactic regimen in uncomplicated cataract surgery.
Source: Jesper Høiberg Erichsen, MD, PhD; Lars M. Holm, MD, PhD; Mads Forslund Jacobsen; JAMA Ophthalmology
doi:10.1001/jamaophthalmol.2021.2976
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


