- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Preoperative Retinal Nerve Fiber Layer Thickness predicts visual functions after Endoscopic Transsphenoidal Surgery for Pituitary Adenoma
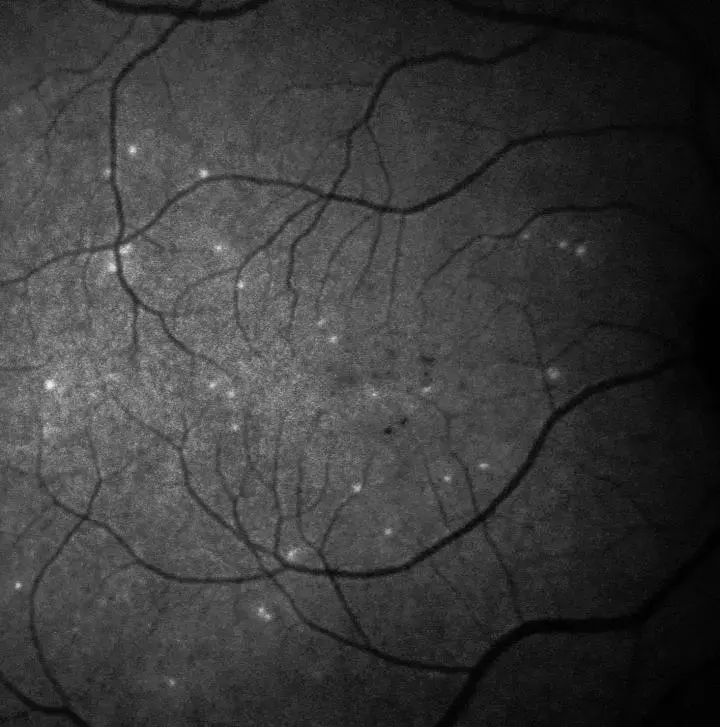 IMAGE: A PATIENT'S RETINA SHOWING HYPERFLUORESCENT SIGNALS - EACH WHITE SPOT IS A SINGLE 'SICK' RETINAL NERVE CELL. IMAGERY SUPPORTED BY DARC TECHNOLOGY USED IN THE PHASE II CLINICAL TRIAL. view more CREDIT: UCL/WESTERN EYE HOSPITAL
IMAGE: A PATIENT'S RETINA SHOWING HYPERFLUORESCENT SIGNALS - EACH WHITE SPOT IS A SINGLE 'SICK' RETINAL NERVE CELL. IMAGERY SUPPORTED BY DARC TECHNOLOGY USED IN THE PHASE II CLINICAL TRIAL. view more CREDIT: UCL/WESTERN EYE HOSPITALPituitary adenomas (PAs) accounts for 10% of intracranial neoplasms. When the PA is larger than 10 mm high, patients may present with visual disturbances due to the compression of the optic chiasm, which located just above the tumor. PA, which is the most common cause of optic chiasm compression, causes axonal damage through disruption of conduction, decreasing axoplasmic flow, demyelination and ischemia from direct compression or stretching of the chiasmatic vessels. The most common indication for surgical treatment of PA is compressive optic chiasmopathy; endoscopic transsphenoidal surgery for pituitary adenoma (ETSS-PA) is the most common surgical technique used for resection of such a tumor.
The factors prognostic of visual recovery after surgical treatment of PA have been studied. Of ophthalmic structural parameters, the loss of peripapillary retinal nerve fiber layer thickness (pRNFLT), measured with optical coherence tomography (OCT), indicates loss of retinal ganglion cell axons resulting from chronic compression of the optic chiasm. There have been various studies supporting the use of pRNFLT as a prognostic factor for postoperative visual recovery after ETSS-PA.
The primary goal of study by Thammakumpee et al was to evaluate the utility of preoperative pRNFLT for predicting postoperative visual functions in terms of their actual values among Thai subjects with PA who were treated with ETSS-PA alone.
This 11-year retrospective study was performed at a single institution in Thailand. Sixty-six eyes of 33 subjects who had a PA compressing the anterior visual pathway and were treated with ETSS-PA alone were included. The pRNFLT was measured globally and in the four quadrants preoperatively, using optical coherence tomography. Multivariable analysis and area under the curve (AUC) were used to demonstrate the prognostic ability of preoperative pRNFLT for postoperative visual functions (> 1 month but < 6 months after ETSS-PA).
The mean postoperative VFI and median postoperative VA were 79.45% ± 24.24% and 0.14 [interquartile range: 0.02, 0.40] logarithm of the minimum angle of resolution.
Among the 56 eyes with a reliable postoperative VFI, thicker preoperative temporal (odds ratio, 1.18; p = 0.024) and inferior (odds ratio, 1.07; p = 0.013) pRNFLT values were associated with a postoperative VFI > 90%.
The strongest association occurred with the preoperative temporal pRNFLT with a cut-off value of 60 µm. Multivariable analysis for all 66 eyes showed that thicker preoperative inferior-quadrant pRNFLT (odds ratio, 1.05; p = 0.001) was associated with a postoperative VA of at least 20/25. The strongest performance was found with the preoperative inferior pRNFLT with a cut-off value of 105 µm.
This study found an association between female sex and favorable VF status (p = 0.014). An earlier medical attention seeking due to PA-related menstrual cycle interruption in females, compared with males, who do not seek medical attention until they have severe hypogonadism or problems due to space-occupying lesions or hypopituitarism, might explain this finding. Study comprehensively established the potential preoperative pRNFLT cut-off values in predicting postoperative VFI > 90% and good postoperative VA within the Thai population. These proposed cut-off values can give ophthalmologists and neurosurgeons enhanced information on postoperative visual prognoses and might, accordingly, help improve preoperative counseling before ETSS-PA. Furthermore, there were significant improvements in postoperative VFI compared with preoperative VFI and postoperative VA compared with preoperative VA.
Postoperative VFI greater than 90% is more likely to be found if the preoperative temporal pRNFLT is greater than or equal to 60 µm, and postoperative VA better than or equal to 20/25 is more likely to be found if preoperative pRNFLT in the inferior quadrant is greater than or equal to 105 µm. These findings provide greater clarity regarding the potential clinical utility of preoperative pRNFLT for predicting postoperative visual functions after ETSS-PA.
Source: Thammakumpee et al; Clinical Ophthalmology 2022:16
https://doi.org/10.2147/OPTH.S392987
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


