- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Quality improvement intervention may help reduce Overuse of Antibiotics in Pediatric Conjunctivitis
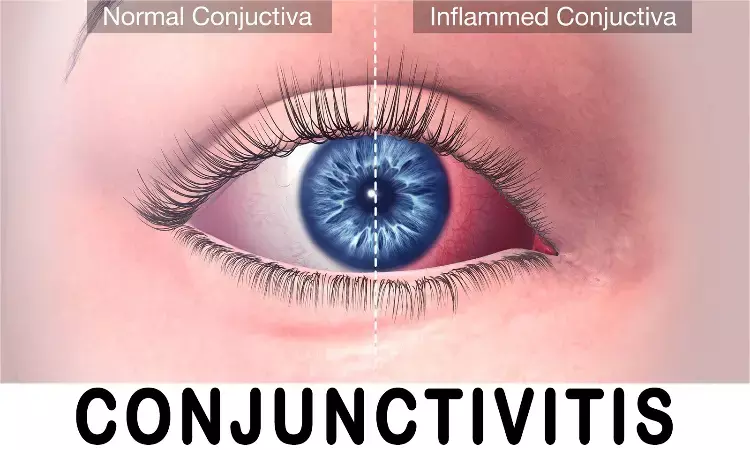
Antibiotics are commonly prescribed for pediatric conjunctivitis, often unnecessarily. However, a recent quality improvement (QI) intervention published in Journal of the Pediatric Infectious Diseases Society has shown promising results in curbing this practice.
The multi-faceted intervention, implemented between November 2018 and December 2022, aimed to reduce unnecessary ophthalmic antibiotic use in children aged 6 months to 17 years with conjunctivitis. This initiative encompassed a clinical care pathway, nurse protocol adjustments, electronic health record (EHR) modifications, parent education materials, and clinician training.
The study, which analyzed data over three time periods: Pre-COVID, Pre-Intervention (November 2018–February 2020); COVID, Pre-Intervention (March 2020–March 2021); and Post-Intervention (April 2021–December 2022), yielded significant results.
Among 6,960 eligible encounters, ophthalmic antibiotic use decreased by a substantial 18.8% from the Pre-COVID, Pre-Intervention period to the Post-Intervention period. During the initial Pre-Intervention period following the onset of the COVID-19 pandemic, a 16.1% reduction in antibiotic use was observed. The implementation of the intervention resulted in an additional 2.7% reduction in antibiotic prescribing, particularly in children aged 6 months to 5 years.
Notably, nurse triage encounters witnessed the most substantial reduction in antibiotic prescribing, with an impressive 82.1% decrease. This marked a dramatic shift from 92.6% antibiotic prescription rates to just 10.5% during nurse triage encounters.
Critically, the study revealed that reducing antibiotic use did not result in an increase in treatment failure rates or healthcare utilization. Treatment failure occurred in 18.7% of cases, with a slightly higher rate (20.0%) among children who received ophthalmic antibiotics compared to those who did not (17.9%).
These findings highlight the success of the QI intervention in Denver, which effectively reduced the unnecessary prescription of ophthalmic antibiotics for pediatric conjunctivitis. Not only does this help prevent overuse of antibiotics, which contributes to antibiotic resistance, but it also demonstrates that judicious use of antibiotics in this context does not compromise the quality of care provided to young patients. This successful intervention in Denver may serve as a model for healthcare systems seeking to improve their antibiotic prescribing practices for pediatric conjunctivitis.
Source:
Sebastian, T., Durfee, J., Wittmer, N., Jack, J., Keith, A., Jenkins, T. C., & Frost, H. M. (2023). Reducing Ophthalmic Antibiotic Use for Non-severe Conjunctivitis in Children. In Journal of the Pediatric Infectious Diseases Society. Oxford University Press (OUP). https://doi.org/10.1093/jpids/piad065
Neuroscience Masters graduate
Jacinthlyn Sylvia, a Neuroscience Master's graduate from Chennai has worked extensively in deciphering the neurobiology of cognition and motor control in aging. She also has spread-out exposure to Neurosurgery from her Bachelor’s. She is currently involved in active Neuro-Oncology research. She is an upcoming neuroscientist with a fiery passion for writing. Her news cover at Medical Dialogues feature recent discoveries and updates from the healthcare and biomedical research fields. She can be reached at editorial@medicaldialogues.in
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


