- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Terson Syndrome-Clinical Presentation, Management, and Visual Outcomes
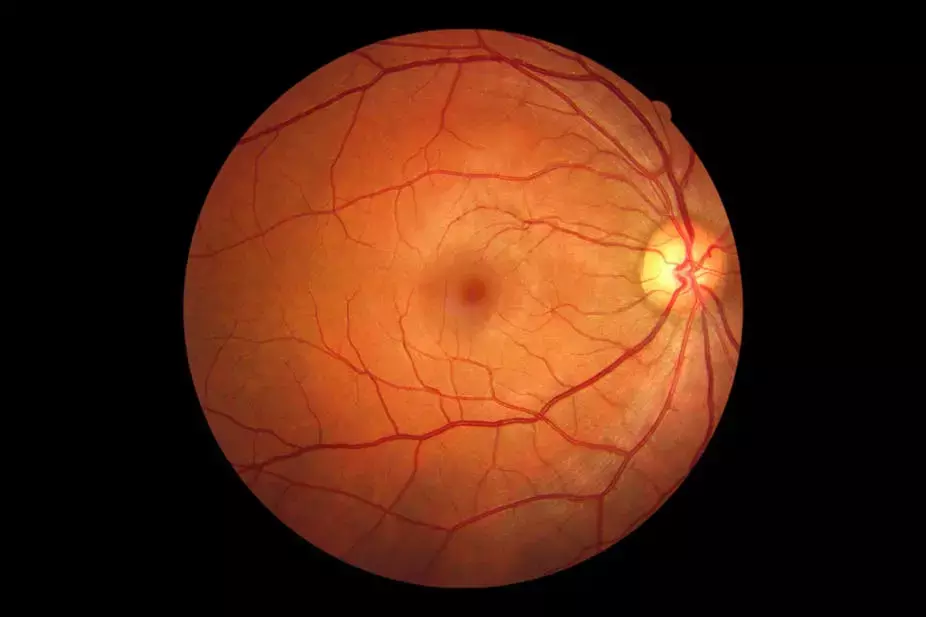
Terson syndrome was first described as an association between subarachnoid haemorrhage and vitreous hemorrhage. This definition has evolved over the years and, nowadays, it comprises various forms of ocular haemorrhage, including vitreous, preretinal, intraretinal, or subretinal bleeding, more commonly identified in patients with intracranial haemorrhage or traumatic brain injury. However, it can also be associated with other causes of acute elevation in intracranial pressure, such as following epidural saline injection, neurosurgical third ventriculostomy, papilledema with development of optociliary shunt vessels and cases of pseudotumor cerebri.
In almost 150 years since its description, the physiopathology of Terson syndrome is still controversial. The most accepted theory is that the sudden increase in intracranial pressure closes the central retinal vein and its choroidal anastomoses, halting venous blood flow from the retina and raising intraluminal pressure within all branches of the vein. When coupled with unimpeded arterial blood flow into the retina, the resultant high intraluminal pressure ruptures the veins and causes bleeding into the retina. Alternative theories suggest that subarachnoid blood may pass into the cerebrospinal fluid surrounding the optic nerve or cause veins within the optic nerve sheath to rupture and then progress through the retinal layers, internal limiting membrane (ILM), and posterior hyaloid membrane, or that subarachnoid blood in skull base cisterns near the optic nerve is refluxed into the globe through glymphatic channels, leading to intraocular hemorrhage.
The diagnosis of Terson syndrome is usually delayed, given the presence of concomitant neurological deficits and depressed conscious state, which limit formal assessment of visual acuity loss. In many patients, ocular haemorrhage resolves spontaneously after a period of observation. If after conservative management, vitreous and/or preretinal haemorrhage does not clear and visual deficits persist, surgical treatment with pars plana vitrectomy (PPV) is recommended. The purpose of this study by Lima-Fontes et al was to characterize the clinical presentation, management strategy and visual outcomes of patients diagnosed with Terson syndrome and followed in a tertiary centre in Portugal.
A single-centre retrospective study was performed, based on the survey review of the medical records of every consecutive patient diagnosed with Terson syndrome and followed from January 2018 to August 2021. The change in best corrected visual acuity (BCVA) from baseline to the final evaluation was the primary outcome.
- Fifteen eyes from 8 patients (50% female) were included. The mean age at diagnosis was 55±7 years. The neurological event was traumatic brain injury in 37.5% (n=3) and subarachnoid haemorrhage in 62.5% of the patients (n=5).
- Bilateral intraocular haemorrhage occurred in 87.5% (n=7) of the patients.
- Vitreous and preretinal haemorrhages occurred each in 66.7% (n=10), intraretinal in 30% (n=3) and subretinal in 13.3% (n=2) of the eyes.
- In 40% of the eyes (n=6), spontaneous resolution of intraocular haemorrhage occurred, while PPV was performed in the remaining 60% (n=9).
- Ocular haemorrhage detection occurred 58.47 ± 40.94 days after the neurological event (range 11 to 121 days).
- Baseline BCVA was 1.11 ± 1.01 logMAR and improved to 0.32 ± 0.69 logMAR in the follow-up period (p=0.004). A positive correlation was found between initial and final BCVA (Spearman’s rho = 0.643, p=0.01). Baseline BCVA of eyes undergoing PPV was lower than of those conservatively managed (1.84±0.72 vs 0.20±0.28 logMAR, p<0.001). However, there were no statistically significant differences in final BCVA after surgery or observation (0.56 ± 0.90 vs 0.04 ± 0.04 logMAR, p=0.149). Longer periods between the neurological and the ophthalmological diagnosis were correlated with worse final BCVA (Spearman’s rho = 0.688, p=0.005).><0.001). However, there were no statistically significant differences in final BCVA after surgery or observation (0.56 ± 0.90 vs 0.04 ± 0.04 logMAR, p=0.149).
Longer periods between the neurological and the ophthalmological diagnosis were correlated with worse final BCVA (Spearman’s rho = 0.688, p=0.005).
In conclusion, Terson syndrome is a potential cause of irreversible visual loss. Evaluation by an ophthalmologist is essential in the initial stages of traumatic brain injury or subarachnoid/intracerebral haemorrhage, particularly if presenting ophthalmologic complaints or depressed neurological status. Early diagnosis permits the adoption of conservative measures and the identification of patients who are more likely to require surgery. PPV is indicated when intraocular haemorrhage is dense and does not resolve spontaneously or when visual acuity at presentation is low, allowing for good visual outcomes with minimal complications. More awareness about Terson syndrome is essential to minimize the diagnosis delay and improve visual outcomes.
Source: Lima-Fontes et al; Clinical Ophthalmology 2023:17 https://doi.org/10.2147/OPTH.S396781
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


