- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
"Orbital imaging - Scanning a patient, reading a disease": An Editorial
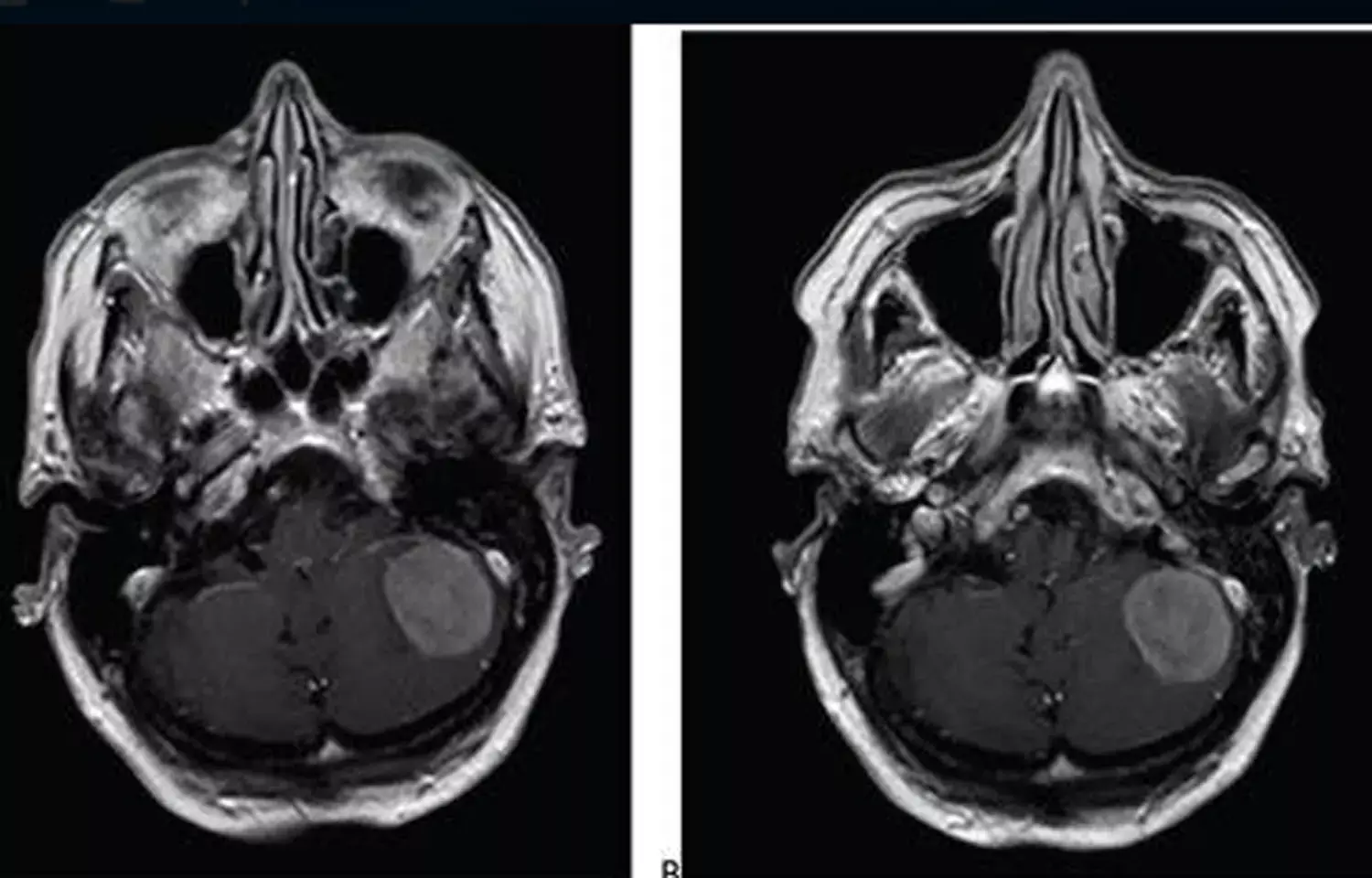
Imaging continues to spook clinicians. Recent advances in imaging and the technical jargon associated with it have made it difficult forthem to even venture to understand it, let alone try interpreting it. Santosh G Honavar in this issue of the Indian Journal of Ophthalmology presented an editorial article on the basics and interpretation of MRI as relevant to an ophthalmologist.
Clinical-radiological correlation is the key to the diagnosis and appropriate management of orbital disorders. The role of an ophthalmologist in orbital imaging includes identification of the optimal imaging tool based on the clinical differential diagnosis, generating a detailed prescription, providing relevant clinical information to the radiologist, interpreting the images, planning management and approach to surgery, and finally, learning from the hindsight of treatment response or histopathological diagnosis if surgery is performed.
Selection and Prescription of Imaging
It is important to select the most appropriate primary imaging modality based on the clinical differential diagnosis. There are specific indications for computed tomography (CT) scan and MRI.
CT scan is preferred as a quick screening modality in a patient with proptosis where the cause is not easily discernible on clinical evaluation. It is also appropriate for patients with orbital trauma with suspected foreign body, orbital fracture, traumatic optic neuropathy (CT of the optic canal with thin sections), orbital cellulitis, acute hemorrhage, optic nerve head drusen, and to rule out retinoblastoma from simulating conditions based on intraocular calcification.
CT scan is indicated for the initial assessment of thyroid eye disease, while additional MRI is indicated to evaluate dysthyroid optic neuropathy.
Baseline CT scan is advised for all suspected orbital infections, inflammations and tumors and is followed by MRI with appropriate parameters where indicted (fungal infection, granulomatous infection/inflammation, specific inflammation, orbital apex syndrome, suspected perineuritis, lesions with possible compressive optic neuropathy, or intracranial extension, and for all tumors where further tissue characterization is considered necessary).
CT scan helps in the evaluation of the orbital bone for preoperative planning of surgical access in orbitotomy and orbital decompression.
Three-dimensional reconstruction of CT scan is ideal for orbital fractures, foreign bodies and contracted socket with bony orbital hypoplasia. CT scan is also indicated in an emergency or if MRI is contraindicated.
Primary MRI is the preferred approach for all neuro-ophthalmic conditions and in a diagnosed case of retinoblastoma to assess choroidal invasion, optic nerve invasion, extraocular extension, intracranial extension, and pineoblastoma.
It is important to image the head and orbit in all neuro-ophthalmic conditions and specifically ask for a detailed study of the brainstem for the evaluation of nystagmus and hemifacial spasm, magnetic resonance angiography (MRA) for hemifacial spasm, and MRI up to second thoracic vertebra and MRA of the neck in Horner's syndrome.
It is also indicated in vascular malformations of the orbit, carotid and duralcavernous fistula, transient monocular vision loss, and third nerve palsy with a suspected aneurism.
Magnetic resonance venography may be indicated in the evaluation of bilateral optic disc edema.
CT or MRI with contrast is advisable in all conditions, except thyroid eye disease and trauma, if not systemically contraindicated
Ophthalmologists must be familiar with MRI protocols and sequences and request as appropriate - fat suppression for post-contrast study for orbital inflammations and tumors, diffusion-weighted imaging for orbital inflammations and tumors and specifically vascular tumors, fluid attenuation inversion recovery for white matter lesions, gradient recall echo for hemorrhage, etc. It is essential to have a constant radiology facility, build a professional relationship and discuss with the radiologist before imaging complex clinical situations, or explain the expected information and leave the decision on MRI protocols to the radiologist.
Interpretation and Clinical-Radiological Correlation
The clinician must learn to interpret CT scans and MRI and indulge in a detailed clinical-radiological correlation before planning the medical management or surgical intervention. If the information provided by imaging fails to meet the requirements for decision-making, does not correlate with the expected pathology or if the imaging shows no abnormality, the clinician must discuss with the radiologist and review the scan together. There would be scope for thinner sections, evaluation with higher magnification, and even re-imaging with a different strategy.
Application of Imaging to Patient Care
The goal of imaging is to optimize patient care. It is used to screen for, exclude and diagnose orbital pathologies, correlate with clinical information and characterize the pathology enough to make a management decision (referral to an expert vs observation vs medical management vs surgery), prognosticate and appropriately counsel the patient, plan the surgical approach and extent (incisional biopsy vs excision), determine the need for intraoperative adjuncts - navigation, rapid intraoperative pathology, etc, plan postoperative adjuvant therapy, and determine the effect of intervention by serial and comparative follow-up scans. Unless the treating clinician is familiar with the scope, strategies and interpretation of imaging, the direct application of imaging to patient care may be suboptimal.
There lies the importance of clinical-radiological-pathological correlation and correlation with the outcome of medical management where histopathology is not available. With such correlation over time and feedback to the radiologist, immense learning can happen within the team and the training environment, imaging protocols can be optimized, interpretation can become more accurate, and plan of treatment can be improved with fewer complications and better patient outcomes.
Source: Santosh G Honavar; Indian Journal of Ophthalmology, Volume 69 Issue 10
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


