- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Revision Acetabular Shell utilized as Tibial Cone in Revision Total Knee Arthroplasty: a case report
One of the biggest challenges of a revision total knee arthroplasty is how to obtain adequate tibial metaphyseal fixation in the setting of significant bone loss. There are multiple implants, including stems, metaphyseal cones, and metaphyseal sleeves, that help provide increased fixation and stability. This report by A. Edelstein et al demonstrates a case in which a porous tantalum metal revision acetabular shell was used as a large tibial cone, as none of the above options were viable due to the size and position of the tibial defect.
A 54-year-old male with past medical history of class 2 severe obesity (BMI 39), chewing tobacco use, and an allergy to penicillins initially presented in 2017 with a chief complaint of left knee pain.
He underwent a left medial unicompartmental knee arthroplasty for left knee medial compartment osteoarthritis. The patient tolerated this procedure well and was recovering without complications until 4 months postoperatively when he was diagnosed with Methicillin-sensitive Staphylococcus Aureus prosthetic joint infection.
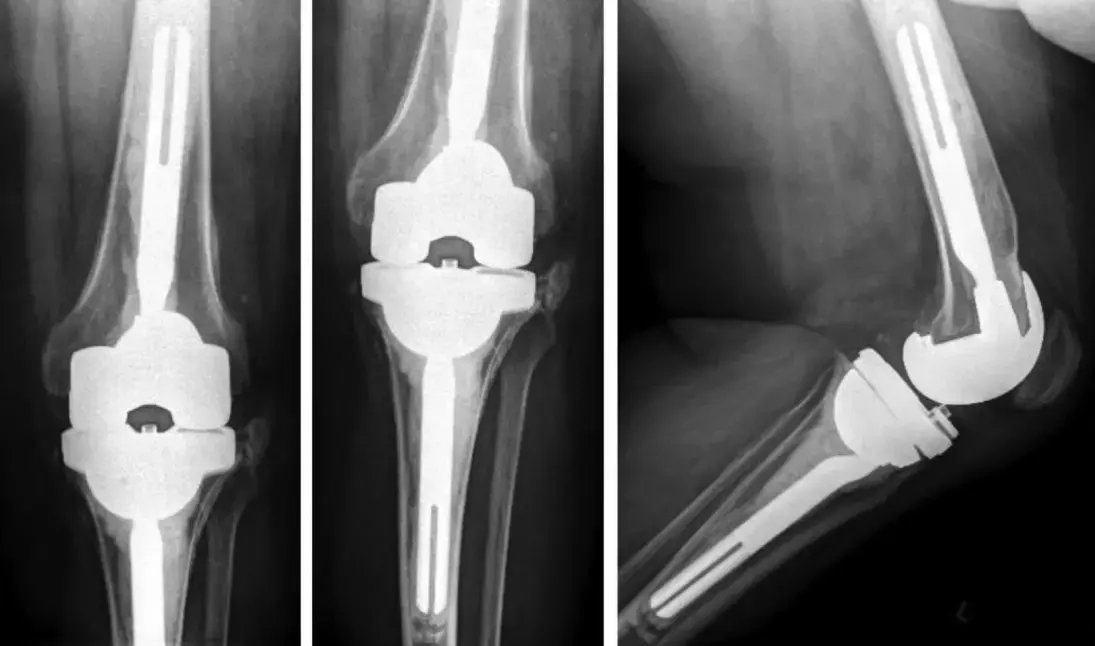
The patient underwent a stage I explantation of the left unicompartmental knee arthroplasty with placement of an antibiotic-laden articulating cement spacer. At the 10-week follow-up visit, the left knee aspiration was negative, and a stage II revision left total knee arthroplasty was performed. Multiple femoral augments were used, and a 31 x 31 x 25-mm trabecular metal tibial cone was used to increase fixation in the setting of a small, contained metaphyseal defect. At his 1-year postoperative visit, the patient was doing well with no reported left knee pain and range of motion (ROM) from 0 to 125 degrees.
Approximately 20 months after the stage II rTKA, the patient presented to the emergency department with a painful and swollen left ankle. A left ankle aspirate grew Methicillin-sensitive Staphylococcus Aureus. In the previous 2 months, he had also been treated for left ankle cellulitis and a nonhealing ulcer on the left second toe. The septic left ankle was successfully treated with arthroscopic irrigation and debridement. The patient then presented 4 months after the ankle washout and debridement with a 2-day history of increasing left knee pain and swelling along with headaches, fevers, and chills.
Aspiration of the left knee was performed, and 30 mL of brown, purulent fluid was obtained. Synovial fluid cultures grew beta-hemolytic streptococci. Given the acute onset of symptoms, his left knee periprosthetic joint infection was treated with a synovectomy, poly-exchange, and intravenous antibiotics.
The left second toe infection had not resolved with antibiotic treatment, and the patient underwent a left second toe amputation for chronic osteomyelitis with podiatry during the same admission. The patient continued to have mild to moderate pain in his left knee, which became acutely worse 6 weeks after the operation. Repeat aspiration demonstrated a nucleated cell count of 28,856 cells/mL. The decision was made to return to the operating room for a 2-stage revision arthroplasty.
He underwent his stage I revision without complications and continued intravenous antibiotics. The revision construct included an antibiotic-laden cement rod that spanned femur and tibia, as well as a static antibiotic cement spacer block.
At 3 months postoperatively, aspiration was negative for bacterial growth, and laboratory values had returned to normal. There was a large contained tibial defect noted after debridement in stage II revision knee arthroplasty. The available porous trabecular metal cones were unable to obtain circumferential purchase in the metaphyseal defect and provide adequate stability. In addition, the largest tibial tray in the revision knee system was not large enough to provide both adequate anterior-posterior (A-P) and medial-lateral (M-L) tibial coverage when trialed with standard, 3-mm, and 6-mm offset stems. The defect was measured to be 50 mm from A-P, 54 mm from M-L, and 25 mm from proximal-distal. This defect was greater in both A-P and M-L diameters than in the available metaphyseal cones and sleeves.
To solve both these issues, the authors opted to use a 54 Trabecular Metal Revision Shell (Zimmer Biomet, Warsaw, IN). The defect was sequentially reamed from 49 mm to 54 mm, which allowed for an adequate circumferential fit, and the implant was placed into the metaphyseal defect with adequate coverage.
A carbide-tipped burr was used to make a small hole at the measured site of stem placement. The shell was then placed into the metaphyseal defect, and the burr was then used to cut out the rest of the slot for the stem and keel in an appropriate position.
After preparation of the tibia the trial components for the femur and tibia were placed and demonstrated excellent collateral balance, and the patella tracked appropriately. The final tibial component with 5-mm augments and a size 16x 135, 6-mm offset splined stem was then inserted. A size 10 condylar constrained poly insert was used.
Intraoperative ROM was 0-130 degrees. The patient was made weight-bearing as tolerated postoperatively with no restrictions on ROM and worked with physical therapy on postoperative day 1. Intraoperative cultures were negative for bacterial growth. Tissue examination demonstrated dense fibrous tissue with dystrophic calcifications.
The patient was seen most recently at 16 months postoperatively with adequate stability and ROM of 5-110 degrees. He reports mild pain in the left knee but is able to ambulate without difficulty.
The authors concluded that – “This case demonstrates that the use of a porous trabecular metal revision acetabular shell can be an additional tool in providing adequate fixation to tibial constructs in the setting of a large contained defect. While this procedure was only performed on 1 patient, we believe that it is an adequate technique that deserves further usage and exploration.”
Further reading:
Utilization of a Revision Acetabular Shell as a Tibial Cone in a Revision Total Knee Arthroplasty Setting
Alexander Edelstein, Michelle Moore et al
Arthroplasty Today 19 (2023) 101095
https://doi.org/10.1016/j.artd.2022.101095
MBBS, Dip. Ortho, DNB ortho, MNAMS
Dr Supreeth D R (MBBS, Dip. Ortho, DNB ortho, MNAMS) is a practicing orthopedician with interest in medical research and publishing articles. He completed MBBS from mysore medical college, dip ortho from Trivandrum medical college and sec. DNB from Manipal Hospital, Bengaluru. He has expirence of 7years in the field of orthopedics. He has presented scientific papers & posters in various state, national and international conferences. His interest in writing articles lead the way to join medical dialogues. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


