- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Childhood Systemic Lupus Erythematosus: IAP Guidelines
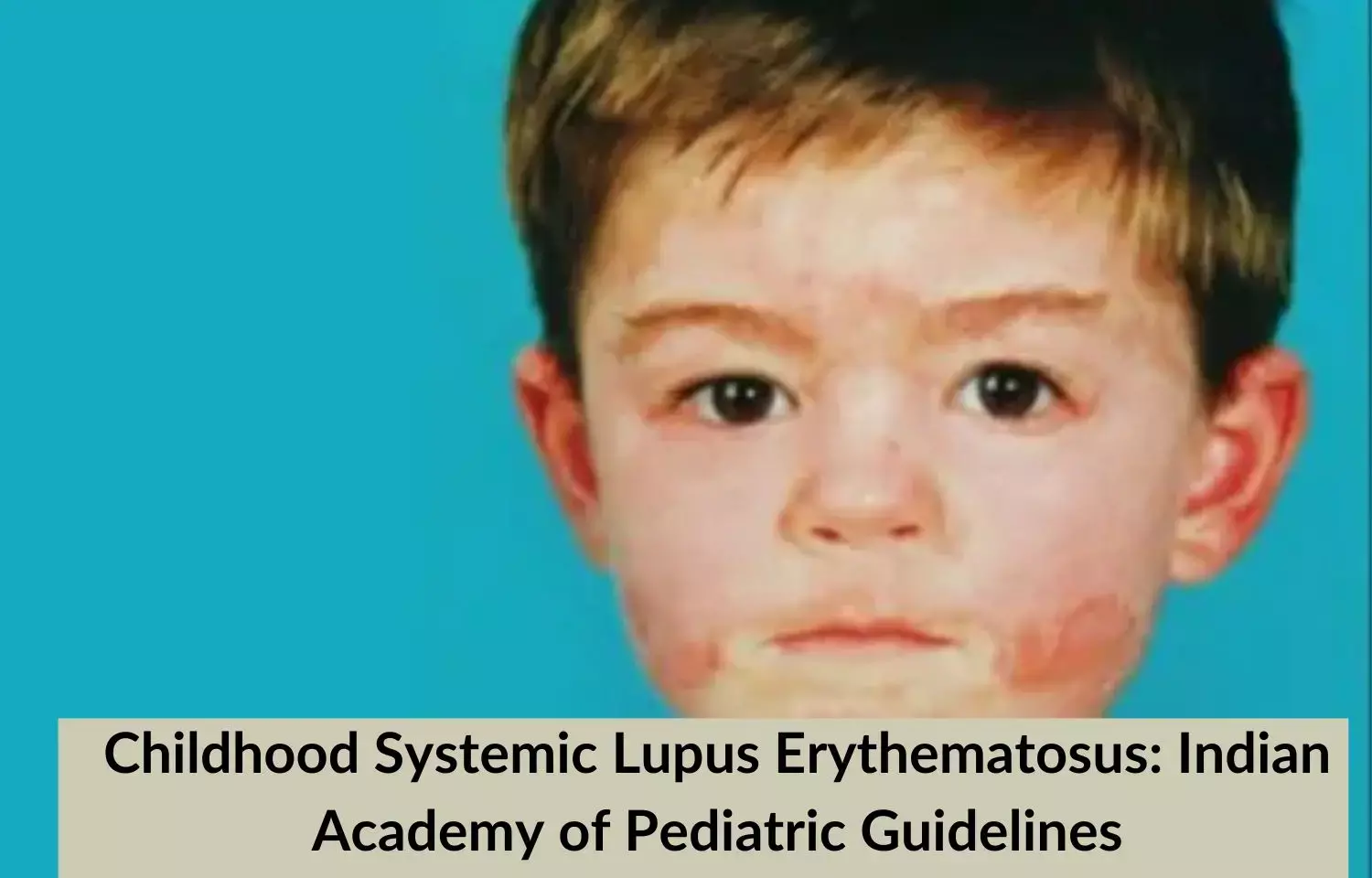
Childhood Systemic Lupus Erythematosus (cSLE) is a chronic heterogeneous autoimmune disease associated with considerable morbidity and significant mortality. It is characterized by multisystem sequential or simultaneous organ involvement (predominant musculoskeletal, cutaneous, renal, hematologic, and neuropsychiatric manifestations) and the presence of antinuclear and other antibodies.
The Indian Academy of Pediatrics (IAP) has released Standard Treatment Guidelines 2022 for Childhood Systemic Lupus Erythematosus. The lead author for these guidelines on Childhood Systemic Lupus Erythematosus is Dr. Nutan Kamath along with co-author Dr. Amit Rawat and Dr. Aaradhana Singh. The guidelines come Under the Auspices of the IAP Action Plan 2022, and the members of the IAP Standard Treatment Guidelines Committee include Chairperson Remesh Kumar R, IAP Coordinator Vineet Saxena, National Coordinators SS Kamath, Vinod H Ratageri, Member Secretaries Krishna Mohan R, Vishnu Mohan PT, and Members Santanu Deb, Surender Singh Bisht, Prashant Kariya, Narmada Ashok, Pawan Kalyan.
Following are the major recommendations of guidelines:
Clinical Manifestations and Classification Criteria for SLE:
The severity of Illness:
Source: Indian Academy of Pediatric Guidelines
Investigations:
| General laboratory investigations | ||
| Erythrocyte sedimentation rate (ESR) | An increase in ESR is in proportion to disease activity. Maybe falsely elevated in hypergammaglobulinemia | |
| Creactive protein |
| |
| Ferritin | Increased, albeit not as much as in macrophage activation syndrome | |
| Specific immunological investigations | ||
| Method of detection | Comments | |
| Antinuclear antibodies (ANA) | Indirect immunofluorescence on HEp2 cells remains the gold standard for detection | Present in more than 90% of children with lupus. Patterns of staining may reflect the antigenic specificity of the antibody |
| Antidouble stranded antibodies (antidsDNA) | Enzyme immunoassay or immunofluorescence |
|
| Complement estimation | Nephelometry or enzyme immunoassay | Complement C3 and C4 are commonly measured. Low levels detected in active disease |
| Extractable nuclear antigens | Can be detected by immunoblotting or by counterimmunoelectrophoresis | Provide useful information on antigenic specificity of ANA |
| Antiphospholipid (aPL) antibodies |
| Positive in a significant proportion of pediatric SLE patients. Anticoagulants (heparin and oral anticoagulants) may interfere with the detection of lupus anticoagulant |
Treatment:
Childhood systemic lupus erythematosus ranges in severity from mild disease with arthritis and rash to devastating nephritis with renal failure or profound neurological disturbances. The approach to therapy is individualized for each patient and based on the clinical features. Nevertheless, treatment is unified based on a few guiding principles.
Ten Principles of Treatment:
1. Treatment by a multidisciplinary team with the pediatric rheumatologist as the Lead
2. Assess organ involvement
3. Assess disease activity and damage index
4. Direct therapy to specific disease manifestations that are active
5. Achieve remission with adequate immunosuppression
6. Therapy for the shortest period and at the lowest possible doses
7. Maintain remission with minimal toxicity of drugs
8. Prompt recognition and aggressive treatment of 'flares' and infection
9. Counsel and educate parents and children
10. Transition to adult care in late adolescence
General Treatment:
Source: Indian Academy of Pediatric Guidelines
Organ-Specific Treatment:
Source: Indian Academy of Pediatric Guidelines
Assess Disease Activity and Damage Index:
Assessment of disease activity and damage is best done by pediatric rheumatologist using the SLE Disease Activity Index (SLEDAI)/British Isles Lupus Assessment Group (BILAG) index and pediatric version of American College of Rheumatology/Systemic Lupus International Collaborating Clinics (ACR/SLICC) damage score index.
Counseling and Education:
- About chronic nature of illness with flares and remissions
- Regular follow-up
- Monitoring for side effects of drugs
- Need for prolonged therapy
- Access to patient information material
- Need for shared care with a multidisciplinary team
- Career choices
- Transition to medical care in late adolescence
- Coping strategies for parents and child
Drugs used in the Management of SLE:
| Name | Dosage | Indications | Important side effects | Monitoring |
| Prednisolone | Initiation of therapy (4–6 weeks): 0.5–2 mg/kg/ day (max 60 mg/day) in at least two divided doses based on type and severity of organ involved. Tapering dose: Reduce by 2.5–5 mg/week till a daily dose of 20 mg Further reduction by 1–2.5 mg every 2–4 weeks till a daily dose of 10 mg After a daily dose of 10 mg is reached, reduce it by 0.5–1 mg every 2–4 weeks | A mainstay of treatment to induce and maintain remission | Obesity, glaucoma, cataract, hypertension, growth suppression, diabetes, osteoporosis, avascular necrosis of bone, infections | Regular blood pressure and random blood sugar monitoring, calcium and vitamin D supplement, bone density monitoring |
| Intravenous pulse methylprednisolone | 10–30 mg/kg to a maximum of 1 g/day for 1–5 consecutive days followed by oral prednisolone as above | Severe cytopenias, proliferative nephritis, major CNS disease, vasculitis, "lupus crisis" | Hypertension, hyperglycemia Rest of the side effects similar to prednisolone | Monitoring of vitals especially blood pressure before starting and during infusion |
| Hydroxy chloroquine | 4–6 mg/kg/day at bedtime (maximum dose 400 mg/day) | Cutaneous disease and adjunct to steroids for systemic disease | Nausea, pruritis, rarely maculopathy | Eye check at starting the drug and biannually for visual acuity, color vision testing, visual field testing, and retinoscopy |
| Methotrexate | 10–15 mg/m2 subcutaneously weekly once |
| GI intolerance, mouth ulcers, alopecia, bone marrow suppression, hepatotoxicity | AST/ALT, serum albumin, CBC at baseline and then at 8–12 weeks intervals |
| Name | Dosage | Indications | Important side effects | Monitoring |
| Nonsteroidal anti inflammatory drugs (NSAIDs) | GI intolerance/ bleed, renal impairment, hypersensitivity | AST/ALT, serum creatinine at baseline and 6-month intervals | ||
| Naproxen | 15–20 mg/kg/day in two divided doses (maximum dose 1 g) | Myalgia, arthralgia, arthritis | Pseudoporphyria pruritis, urticarial, morbilliform rash, erythema multiforme | |
| Ibuprofen | 30–40 mg/kg/day in three divided doses (maximum dose 2.4 g) | Positive aPL antibodies | ||
| Aspirin | 3–5 mg/kg/day | |||
| Cyclophosphamide | 1–2 mg/kg/day (PO) or 500–1000 mg/m2/month (IV) in severe disease | Severe cytopenias, proliferative nephritis, major CNS disease, vasculitis | Nausea, vomiting, cytopenias, infections, hemorrhagic cystitis | Ensure adequate fluid intake CBC on days 7 and 14 if on pulse therapy |
| Azathioprine | 0.5–2.5 mg/kg/day (PO) (Maximum 150 mg/day) | Mild SLE unresponsive to glucocorticoids and HCQS or develop unacceptable drug toxicity | Cytopenias, pancreatitis Opportunistic infections | CBC monthly and after dose increments, hepatic enzymes, BUN, creatinine amylase, and lipase at the onset of treatment and every 3 months |
| Mycophenolate Mofetil | 1200–1800 mg/ m2/day twice daily (PO) (Maximum 3000 mg/day) | Induction and maintenance of severe cytopenias, vasculitis, proliferative and membranous nephritis, steroid sparing in moderate to severe illness |
þ Pancytopenia
| CBC every 8–12 weeks |
| Name | Dosage | Indications | Important side effects | Monitoring |
| Cyclosporine A | 2.5–5 mg/kg/day | Membranous nephropathy | nephrotoxic | Blood urea nitrogen, creatinine, urine analysis, hepatic enzymes, CBC at start of therapy and monthly |
| IV Immuno globulin | Up to 2 g/kg | Severe thrombocytopenia, catastrophic antiphospholipid syndrome | Anaphylaxis, Aseptic meningitis (Headache, vomiting 18–36 hours after the infusion) | Monitor blood pressure and pulse rate every 15 minutes for the first hour, every 30 minutes for the second hour, and every hour thereafter |
| Rituximab | 375 mg/m2/week intravenously (four doses at intervals of 7 days) OR 750 mg/m2 ( two doses at intervals of 14 days) | Severe and refractory disease | Infection Hypogamma globulinemia Infusion reaction | Monitor CBC at the start of therapy |
| Belimumab (approved for children > 5 years) | 10 mg/kg every 4 weeks | Clinically active disease without severe nephritis or neuropsychiatric lupus | Infection | Monitor CBC at the start of therapy and monthly |
(CBC: complete blood count; ALT: alanine transaminase; AST: aspartate aminotransferase)
- Complications:
Source: Indian Academy of Pediatric Guidelines
Role of General Pediatrician (GP):
Source: Indian Academy of Pediatric Guidelines
Prognosis:
Early diagnosis and appropriate therapy ensure a good prognosis. Intercurrent infections, flares, renal and cardiovascular disease, neurologic manifestations, and poor adherence to treatment affect the outcome. The morbidity of the disease and adverse effects of the medications must be minimized to achieve a satisfactory long-term outcome.
Neonatal Lupus:
Source: Indian Academy of Pediatric Guidelines
Drug-induced Lupus:
Source: Indian Academy of Pediatric Guidelines
Lupus Mimics:
| Infections | |
| Viral | EpsteinBarr virus, Cytomegalovirus, Parvovirus B19, Human Herpes Virus 6 |
| Bacterial | Brucellosis, Leptospirosis, Q fever, Mycoplasma |
| Spirochetal | Lyme disease |
| Protozoal | Toxoplasmosis |
| Malignancy | Leukemia, Lymphoma |
| Other autoimmune diseases | Mixed connective tissue disease, systemic vasculitis, antiphospholipid syndrome, juvenile dermatomyositis |
Summary:
Diagnosis and management of cSLE is a challenge due to its myriad clinical presentations. Shared care pathways between specialists from different disciplines and different levels of care (primary, secondary, and tertiary) are of paramount importance in the management of cSLE.
Reference:
- Aringer M, Costenbader K, Daikh D, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71(9):1400-12.
- Gergianaki I, Bertsias G. Systemic lupus erythematosus in primary care: an update and practical messages for the general practitioner. Front Med (Lausanne). 2018;5:161.
- Groot N, de Graeff N, Marks SD, Brogan P, Avcin T, Bader-Meunier B, et al. European evidence-based recommendations for the diagnosis and treatment of childhood-onset lupus nephritis: the SHARE initiative. Ann Rheum Dis. 2017;76(12):1965-73.
- Massias JS, Smith EMD, Al-Abadi E, et al. Clinical and laboratory characteristics in juvenile-onset systemic lupus erythematosus across age groups. Lupus. 2020;29(5):474-81.
- Trindade VC, Carneiro-Sampaio M, Bonfa E, Silva CA. An update on the management of childhood-onset systemic lupus erythematosus. Paediatr Drugs. 2021;23(4):331-47.
- The guidelines can be accessed on the official site of IAP:https://iapindia.org/standard-treatment-guidelines/
I have done my Bachelor of pharmacy from United Institute of Pharmacy and currently pursuing pharmaceutical MBA from Jamia hamdard. I worked as an intern at the position of content creator in Medical Dialogue and am highly obliged to the company for giving me this wonderful opportunity.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


