- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Laryngeal control therapy reduces need for asthma drugs in kids with PVFMD: Study
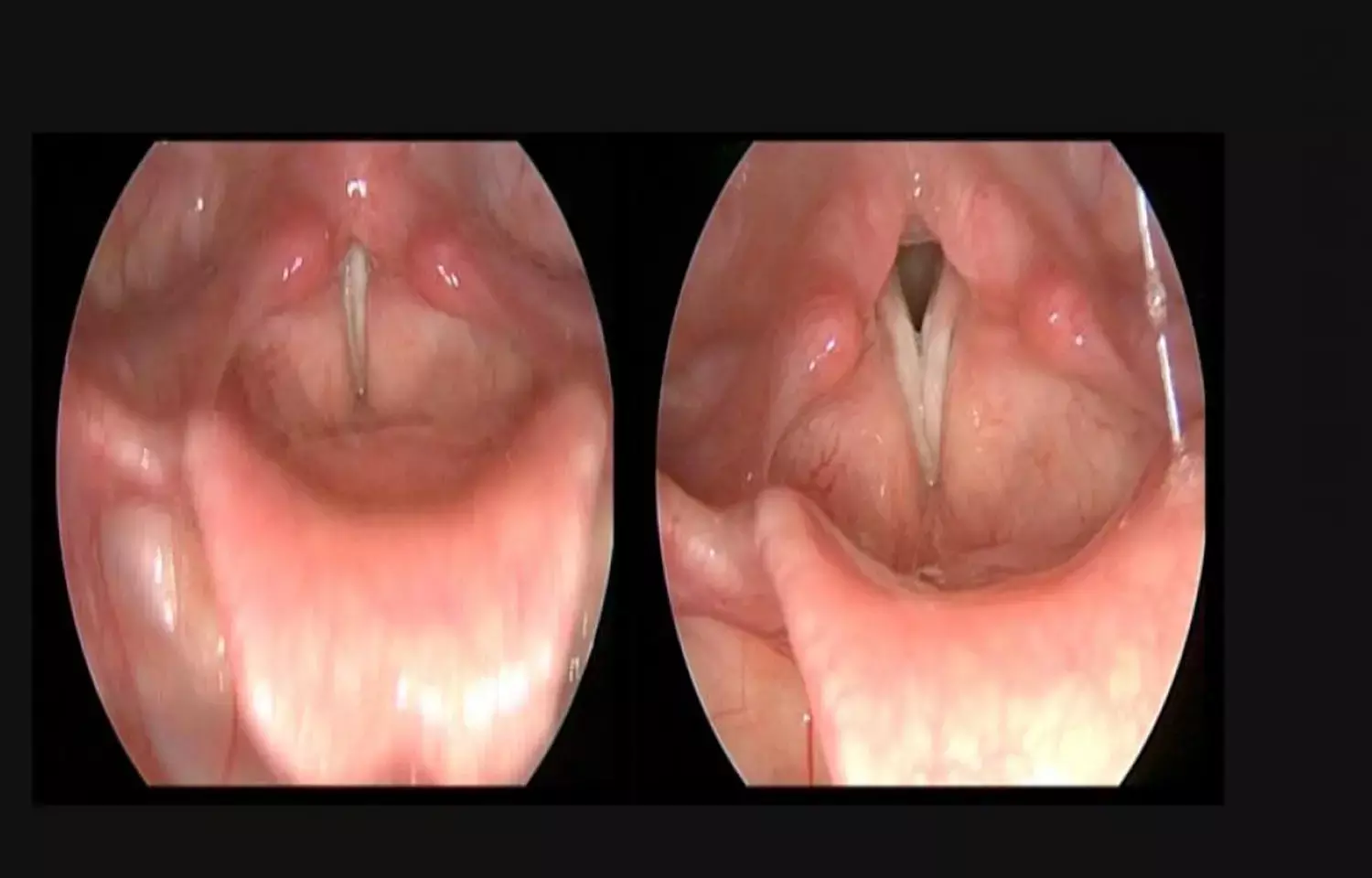
USA: Participation in laryngeal control therapy (LCT) reduces the use of asthma medication in pediatric patients with paradoxical vocal fold motion disorder (PVFMD), finds a recent study in the journal The Laryngoscope. LCT consists of teaching breathing techniques and identification of physical, emotional and environmental contributing factors and strategies for their reduction.
According to the study, LCT for pediatric PVFMD leads to a significant decrease in symptoms as measured by the Dyspnea Index (DI).
Brad deSilva, The Ohio State University Wexner Medical Center, Columbus, Ohio, U.S.A., and colleagues conducted this prospective observational study to determine if the diagnosis and treatment of PVFMD leads to decreased use of asthma medication. They also determined dyspnea outcomes following diagnosis and treatment for PVFMD.
The researchers recruited 26 patients (aged 11 to 17 years) with newly diagnosed PVFMD. They were required to fill a medication questionnaire and Dyspnea Index at the initial visit, at the first return visit, and at greater than 6 months post‐diagnosis and therapy.
Key findings of the study include:
- There were 19/26 (73%) patients diagnosed with asthma prior to a diagnosis of PVFMD, and 26/26 (100%) patients were using an inhaler prior to the enrollment visit.
- Twenty‐two (85%) patients completed follow‐up questionnaires.
- Five patients participated in no therapy, seven patients in partial therapy, and 14 patients in full therapy.
- Significant reduction in asthma medication use was seen in the full therapy group and in those with exercise as their only trigger.
- Furthermore, symptoms as scored by the DI decreased overall from 25.5 to 18.8.
"Diagnosis and treatment of pediatric PVFMD leads to a decline in asthma medication use in those patients who participate in at least two LCT sessions and in those with exercise‐induced PVFMD," concluded the authors.
The study, "Reduced Asthma Medication Use after Treatment of Pediatric Paradoxical Vocal Fold Motion Disorder," is published in the journal The Laryngoscope.
DOI: https://onlinelibrary.wiley.com/doi/abs/10.1002/lary.29283
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


